Adverse psychosocial work stressors, such as job strain (1), effort–reward imbalance (ERI) (2), and organizational injustice (3) have been linked to impaired employee health and an increased risk of chronic diseases (4–9). These partially overlapping stressors capture various psychosocial characteristics of the work, workplace, and workers’ perceptions. Job strain refers to a combination of high job demands and low job control (1) whereas ERI concerns the possible imbalance between efforts an employee makes at work and the rewards (eg, salary, promotion prospects, esteem or job security) s/he gains (2). Organizational injustice, in turn, refers to a situation in which an employee perceives the organization’s decision-making processes to be unfair and/or feels to be mistreated by his/her supervisor (3). Distributive justice, a further dimension of organizational justice not considered in this study, evaluates the fairness of exchange.
Recent meta-analyses on observational cohort studies have shown that all three stressors – job strain, ERI and organizational injustice – are associated with an increased risk of depressive disorders (4, 8), ischemic heart diseases (5), diabetes (9) and musculoskeletal diseases (6, 7). Previous studies have also shown a relationship between high levels of job strain, ERI and organizational injustice and an increased risk of all-cause disability pension (10–15), and disability pension due to depressive or musculoskeletal disorders (10, 11, 14). A limitation in previous studies is that the focus has almost exclusively been on single stressors, although the health effects may vary between specific stressors and co-occurring stressors. Multiple stressors (ie, repeated hits from various stressors) may potentially be associated with more harmful effects on employee health and work ability than single stressors (16, 17), which may be more easily adapted. Supporting this reasoning, a recent multi-cohort study found that the combination of job strain and ERI was associated with a 40% higher risk of coronary heart disease while the excess risk for these stressors separately was only 16%, compared to those with no work stressors (18). Few longitudinal studies have examined whether the three work stressors cluster (ie, occur together more often than expected by chance) and whether the effect of co-occurring work stressors on disability retirement is different from single work stressors. Furthermore, it is not known if a specific combination of these stressors is particularly harmful for work ability. Information on these issues has potentially important implications for prevention of early labor market exit.
We have previously studied job strain, ERI, and organizational injustice separately in association with all-cause and diagnosis-specific disability pension in the Finnish Public Sector (FPS) study (10, 11, 14). In the present prospective study from the same cohort, we used updated data to examine the extent to which these three major work stressors cluster and whether specific combinations of co-occurring work stressors are particularly strongly related to the risk of disability pension due to any cause and disability from depressive or musculoskeletal disorders, the two most common causes of disability retirement (19, 20). In addition to work stressors measured by individual survey responses, we used work-unit aggregates of work stressors, assigned to every member of the work-unit eligible to the survey, as a more objective measure of the exposure to reduce reporting bias (10, 21).
Methods
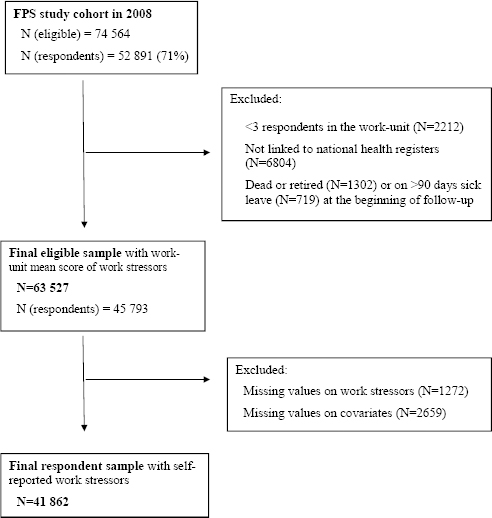
The present study utilized the FPS study cohort, which includes all employees who have worked full-time (or full- or part-time in hospital districts) for ≥6 months in the participating organizations (ten towns and six hospital districts). The Ethics Committee of the Hospital District of Helsinki and Uusimaa has approved the FPS study. The eligible population for this study comprised those employees who had a work contract for ≥6 months in one of the target organizations in 2008 (N=74 564) (figure 1). Of this eligible population, 52 891 had responded to the 2008 FPS study survey (response rate 71%) including questions on job strain, ERI, and organizational injustice. These survey responses were used to calculate a work-unit-based aggregate score of work stressors for each eligible study participant (either respondent or non-respondent). Of the 74 564 eligible participants, we excluded those working in work units with <3 respondents (N=2212). Of the remaining employees, 65 548 had earlier been linked to national health registers. Of these, we excluded those who had died or retired (N=1302) or were on a long (>90 days) sick leave (N=719) at the beginning of the follow-up, which was the date of survey response in 2008. Thus, the final study sample comprised 63 527 eligible employees and 45 793 survey respondents. Finally, of the survey respondents, we excluded those with missing values on job strain, ERI or organizational injustice (N=1272) or any baseline covariate (N= 2659). Thus, the final sample of survey respondents comprised 41 862 employees.
Work stressors
Exposure to job strain, ERI, and organizational injustice was measured from surveys similarly as in our previous studies (10, 11, 14). Briefly, job demands and control were measured with 12 items derived from the Job Content Questionnaire (1). The mean of job control scores (9 items) was subtracted from the mean of demand scores (3 items) to measure the job strain score (22, 23). As earlier, we used a 4-item scale measuring efforts with one question and rewards with three questions as a proxy for ERI (10, 24). The remainder from the ratio of efforts and rewards (ie, effort score/ mean of reward scores) was used as an ERI score. The 4-item proxy scale has a relatively high correlation (R=0.6) with the 10-item version of the standard ERI scale (10). The procedural and relational justice were measured with the original 13-item scale (25), and the organizational justice score was calculated as the mean of procedural and relational justice [ie, (mean of 7-item procedural justice + mean of 6-item relational justice)/2] (26). There was no substantial overlap between the stressors (all correlation coefficients <0.30). The highest quartile of job strain and ERI and lowest quartile of organizational justice indicated exposure to each psychosocial stressor, while the remaining three quartiles of each stressor were set as non-exposed. An 8-category variable was created to measure all the possible combinations of the three psychosocial stressors: (i) non-exposed, (ii) strain only, (iii) ERI only, (iv) injustice only, (v) strain+ERI, (vi) strain+injustice, (vii) ERI+injustice, and (viii) strain+ERI+injustice. Categories were exclusive, thus each participant belonged to one category only.
In addition to self-reported exposure, we calculated work-unit aggregates, as in our previous studies, to measure work stressors more objectively (ie, independently from individual characteristics) (10, 11, 14, 21). A work-unit aggregate was calculated for each psychosocial stressor as a mean value of all responses within the same work unit for work units with ≥3 respondents and assigned for each participant in that work unit. The correlation coefficients of aggregated stressors varied between 0.11−0.32. Similarly as for the self-reported exposure, the most unfavorable quartile was chosen as the exposure. The intra-class correlation for aggregated job strain was 16%, 4% for aggregated ERI, and 18% for aggregated organizational injustice, suggesting significant variance in job strain and organizational injustice between work units, and low within work-unit resemblance of individual answers to ERI.
Disability pension
We obtained information from the national pension records held by the Finnish Centre for Pensions. These nation-wide pension data were available for all participants regardless of their employment status or workplace at the follow-up. The starting dates and main diagnoses according to International Classification of Diseases, 10th Revision (ICD-10) were retrieved on all full-time or partial disability pensions (permanent or fixed-term). All-cause disability pension and disability pension due to the two most common causes of disability retirement – depressive disorders (ICD-10 codes F32-F34) and musculoskeletal disorders (ICD-10 codes M00-M99) – were chosen as study outcomes (10, 11, 14, 19, 20). The data were obtained for disability pensions granted after the start of the follow-up until 31 December 2011.
Covariates
Sociodemographic factors were derived from the employers’ registers and included age, sex, the geographical location of the workplace (Northern, Southern or Central Finland) and occupational status. Occupational status was categorized according to the classification of occupations by the Statistics Finland (27) into higher non-manual, lower non-manual and manual. The level of education (primary, secondary or tertiary) was obtained from the records of Statistics Finland.
A history of physical illnesses (yes/no) and/or mental disorders (yes/no) was determined using data from various national registers. History of physical illnesses was coded “yes” if any of the following criteria was met: entitlement, effective at the beginning of the follow-up, to special reimbursement for the costs of medication for diabetes, asthma, chronic obstructive pulmonary disease, hypertension, cardiac insufficiency, or coronary heart disease; a record of cancer diagnosis; or purchases equal to >100 defined daily dosages (DDD) of prescribed pain killers during the five years preceding the beginning of the follow-up. History of mental disorder was coded “yes” if any of these conditions was fulfilled: entitlement (effective at the beginning of the follow-up) to special reimbursement of antipsychotic medication; long-term sickness absence (>90 days) or hospitalization due to mental disorders (ICD-codes F00-F99), reimbursed psychotherapy, and purchases (>100 DDD) of prescribed antidepressant medication during the five years before the beginning of the follow-up. Eligibility to special reimbursement for the costs of medication is granted by application (ie, statement from a physician) to all patients diagnosed with diabetes (type 1 or 2), cardiac insufficiency, asthma, coronary heart disease or psychotic disorders (such as schizophrenia, psychotic depression or bipolar depression). However, concerning chronic obstructive pulmonary disease and hypertension, the eligibility for the special reimbursement is stricter than indications to use medication for these diseases (28).
Behavior-related risk factors were derived from the baseline survey requesting information on smoking status (current smoker/ non-smoker), high alcohol intake (yes/no), obesity (yes/no), and sedentary lifestyle (yes/no). Alcohol abuse was coded “yes”, if average absolute alcohol consumption was >210g per week. If self-reports of height and weight resulted in body mass index (BMI) of ≥30 kg/m2, the participant was coded as obese. Leisure-time physical activity <2.0 metabolic equivalent task (MET) hours per day (corresponding to approximately 30 minutes of walking) meant that participant had a sedentary lifestyle (29).
Statistical analysis
We used two samples: the survey respondents and eligible employees. For the survey respondents, we first calculated the rate of disability pension / 1000 person years by their baseline characteristics. For both samples, we studied the extent to which work stressors were clustered. The observed prevalence of each risk factor was the percentage of the sample reporting that risk factor. Expected prevalence for each combination of work stressors, assuming no association between the stressors (ie, independence), was calculated by multiplying the observed prevalence of each stressor (30). A measure of clustering was calculated as observed divided by expected (O/E) prevalence for each work stressor combination. Confidence intervals (CI) were obtained through bootstrapping procedures. Clustering was determined to have occurred when the 95% CI for the O/E did not include one (30).
Cox proportional hazard marginal models were used to examine the association between the combined variables of work stressors and disability pensioning. To take into account the nested structure of the data, workplace was used as the cluster variable. Because disability pensions are relatively rare and aggregated stressors were based on work units, we used employer (town, hospital district) as a cluster variable (N=16). Those with no work stressors acted as a reference group. The follow-up began from the date of survey response in 2008 and ended (i) if the participant was granted disability pension (study end-point) or old age pension, (ii) if s/he died, or (iii) on 31 December 2011, whichever came first. The models for the survey respondents were first adjusted for age, sex and region (geographical location of workplace) (model 1), then additionally also for occupational status, education, baseline physical and mental health, and behavior-related risk factors (obesity, smoking and high alcohol consumption) (model 2). Model 1 for the eligible population with work-unit aggregated exposure was similar to that of the survey respondents, model 2 was additionally adjusted for education and baseline physical and mental health. The cumulative incidence of disability pension due to any cause and depressive and musculoskeletal disorders by each category of self-reported exposure from age 30–63 years (the most common statutory retirement age) was studied with Kaplan-Meier estimator. All results were expressed as hazard ratios (HR) and their 95% CI. The SAS statistical software version 9.4 (SAS Institute Inc, Cary, NC, USA) was used in all analyses.
Results
Most (80%) of the participants were women and worked in Southern Finland (56%) (table 1). Over half of the study population had tertiary education (60%) and half of them were in lower non-manual jobs (51%). The highest rates of disability pension were observed for those who (i) were aged 50–60 years, (ii) were employed in manual jobs, (iii) had primary education only and (iv) had physical or mental illnesses.
Table 1
Participant characteristics and the rate of disability pension.
Half of the participants were not exposed to any of the work stressors, about a quarter were exposed to 1 stressor, one fifth to a combination of any 2 stressors and around 5% to all 3 stressors (table 2). The 3 stressors were clustered so that the observed prevalence of having 0 or 2–3 stressors was significantly higher than expected, and the observed prevalence of having only 1 stressor was significantly lower than expected. The highest O/E ratio was observed for having all 3 work stressors both in the eligible population and among the survey respondents [O/E 2.6 (95% CI 2.5–2.7) and 3.9 (95% CI 3.7–4.0), respectively].
Table 2
Clustering of job strain, effort−reward imbalance (ERI) and injustice. Observed prevalence and observed/expected (O/E) prevalence ratio and their 95% confidence intervals (CI) for all combinations of the stressors. [+ = presence of risk factor; - = absence of risk factor].
| Stressors (N) | Work stressora | Eligible population (N=63 527) | Respondents (N=41 862) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Strain | ERI | Injustice | Observed | O/E | 95% CI | Observed | O/E | 95% CI | |
| 0 | - | - | - | 50.8 | 1.21 | 1.20–1.21 | 51.1 | 1.24 | 1.23–1.25 |
| 1 | + | - | - | 8.6 | 0.61 | 0.60–0.62 | 9.0 | 0.64 | 0.63–0.66 |
| 1 | - | + | - | 7.5 | 0.53 | 0.52–0.54 | 9.3 | 0.62 | 0.61–0.64 |
| 1 | - | - | + | 11.3 | 0.81 | 0.80–0.82 | 9.4 | 0.69 | 0.68–0.71 |
| 2 | + | + | - | 8.1 | 1.73 | 1.70–1.77 | 6.0 | 1.18 | 1.14–1.21 |
| 2 | + | - | + | 4.3 | 0.91 | 0.88–0.93 | 4.0 | 0.87 | 0.83–0.90 |
| 2 | - | + | + | 5.3 | 1.14 | 1.11–1.17 | 4.9 | 1.00 | 0.97–1.04 |
| 3 | + | + | + | 4.1 | 2.59 | 2.51–2.68 | 6.4 | 3.85 | 3.73–3.97 |
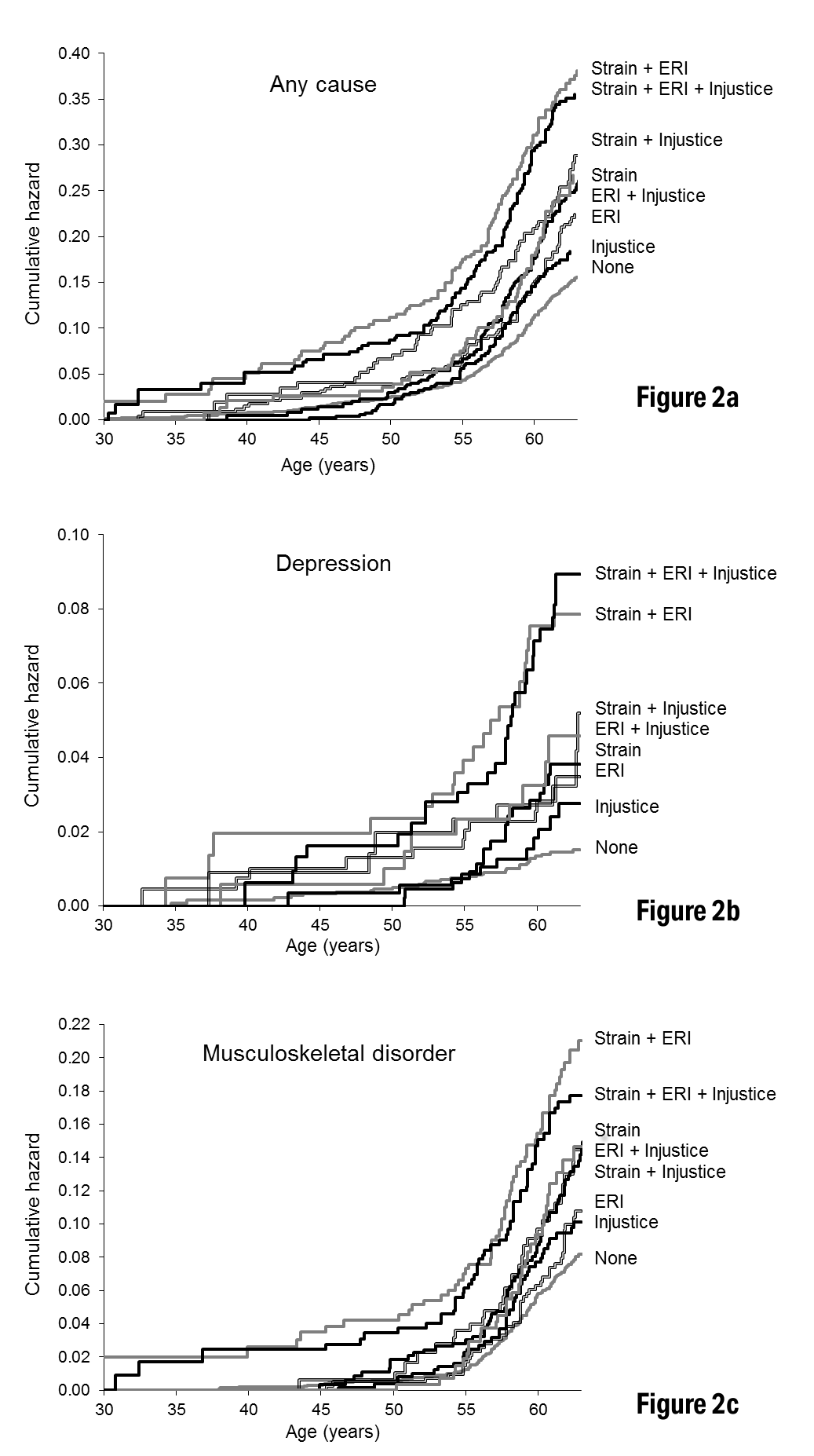
During a mean 3.1 years of follow-up, altogether 1678 (2.6%) eligible participants and 976 (2.3%) survey respondents were granted a disability pension. figure 2 shows the cumulative hazard curves of disability pension by categories of self-reported work stressors for ages 30–63 years. The dispersion of hazard curves of all-cause disability pension was observed from the 45 years of age onward (figure 2a). By the age of 63 years, 15% of the employees who were not exposed to any of the stressors had ended up on disability pension. Among those exposed to both job strain and ERI, one fifth of the employees had retired due to a disability by the age of 57 years, while – by the age of 63 – this proportion was almost 40%. The cumulative hazard curves of disability pension due to depressive disorders are illustrated in figure 2b and those of disability pension due to musculoskeletal disorders in figure 2c.
Figure 2
Cumulative hazard curves of all-cause and diagnosis specific disability pension by combinations of self-reported work stressors. [ERI=effort−reward imbalance.]
Clusters of self-reported work stressors and disability pension
Table 3 shows the risk of disability pension for different combinations of self-reported strain+ERI+injustice compared to the non-exposed. Adjusted for demographics and region, the risk of all-cause disability pension was elevated for all stressor categories. The highest risk was observed for the clusters of work stressors, especially the combination of strain+ERI and strain+ERI+injustice [HR 2.8 (95% CI 2.3–3.4) and 2.5 (2.2–2.9), respectively]. Further adjustment for education, occupational status, baseline physical and mental health and health behavior-related risk factors attenuated the observed associations by 39–52%. The risks for the clusters of work stressors remained above that of single stressors and were highest for the strain+ERI and strain+ERI+injustice combinations [HR 2.1 (95% CI 1.8–2.6) and 1.9 (1.7–2.2), respectively]. For strain, ERI and injustice only, the corresponding HR were 1.5 (95% CI 1.2–1.8), 1.2 (95% CI 1.0–1.5) and 1.2 (95% CI 0.9–1.4).
Table 3
Combinations of self-reported work stressors and risk of disability pensiona. Finnish Public Sector study respondents to 2008 survey (N=41 862) were followed until the end of 2011. [CI=confidence interval; ERI=effort−reward imbalance; HR=hazard ratio.]
| Measurement, combination of stressors | Participants | Cause of disability pension | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Any cause (N=976) | Depression (N=136) | Musculoskeletal (N= 488) | ||||||
|
|
|
|
||||||
| N | % | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Model1b | ||||||||
| None | 21 379 | 51.1 | 1.00 | 1.00 | 1.00 | |||
| Strain only | 3768 | 9.0 | 1.73 | 1.43–2.11 | 2.67 | 1.73–4.12 | 1.68 | 1.33–2.13 |
| ERI only | 3875 | 9.3 | 1.45 | 1.19–1.78 | 2.16 | 1.28–3.62 | 1.28 | 1.05–1.57 |
| Injustice only | 3943 | 9.4 | 1.26 | 1.00–1.59 | 1.97 | 1.11–3.51 | 1.25 | 1.00–1.57 |
| Strain + ERI | 2492 | 6.0 | 2.78 | 2.30–3.35 | 5.35 | 3.29–8.70 | 2.57 | 2.18–3.02 |
| Strain + Injustice | 1674 | 4.0 | 1.93 | 1.49–2.50 | 2.98 | 1.62–5.47 | 1.71 | 1.27–2.29 |
| ERI + Injustice | 2051 | 4.9 | 1.83 | 1.38–2.42 | 3.22 | 1.78–5.84 | 1.94 | 1.44–2.61 |
| Strain + ERI + Injustice | 2680 | 6.4 | 2.53 | 2.24–2.86 | 6.45 | 4.24–9.83 | 2.17 | 1.73–2.72 |
| Model 2c | ||||||||
| None | 21 379 | 51.1 | 1.00 | 1.00 | 1.00 | |||
| Strain only | 3768 | 9.0 | 1.45 | 1.18–1.77 | 2.47 | 1.52–4.01 | 1.30 | 1.01–1.67 |
| ERI only | 3875 | 9.3 | 1.22 | 1.00–1.48 | 1.87 | 1.11–3.17 | 1.07 | 0.87–1.32 |
| Injustice only | 3943 | 9.4 | 1.16 | 0.94–1.43 | 1.66 | 0.97–2.85 | 1.19 | 0.96–1.48 |
| Strain + ERI | 2492 | 6.0 | 2.12 | 1.75–2.57 | 4.40 | 2.43–7.96 | 1.87 | 1.54–2.26 |
| Strain + Injustice | 1674 | 4.0 | 1.53 | 1.20–1.96 | 2.30 | 1.23–4.31 | 1.32 | 0.98–1.77 |
| ERI + Injustice | 2051 | 4.9 | 1.49 | 1.09–2.05 | 2.38 | 1.30–4.34 | 1.62 | 1.15–2.28 |
| Strain + ERI + Injustice | 2680 | 6.4 | 1.90 | 1.66–2.18 | 4.70 | 2.86–7.70 | 1.61 | 1.32–1.97 |
Table 3 also shows the risk of disability pension due to depressive disorders for the combinations of self-reported psychosocial stressors compared to the non-exposed. Adjusted for demographics and region, the HR varied between 2.0–2.7 (95% CI 1.1–4.1) for the single stressors and between 3.0–6.5 (95% CI 1.6–9.8) for their different combinations. These associations attenuated by 10–19% in the fully adjusted models. The highest risks were observed for the strain+ERI and strain+ERI+injustice combinations [HR 4.4 (95% CI 2.4–8.0) and 4.7 (95% CI 2.9–7.7), respectively].
The last column of table 3 shows the associations between combinations of self-reported work stressors and risk of disability pension due to musculoskeletal disorders compared to the non-exposed. Adjusted for demographics and region, this risk was elevated for all stressor categories except organisational injustice alone.
Again, highest risk was observed for the clusters of work stressors, especially the combination of strain+ERI and strain+ERI+injustice [HR 2.6 (95% CI 2.2–3.0) and 2.2 (1.7–2.7), respectively], while for the single stressors the HR varied between 1.3–1.7 (95% CI 1.0–2.1). These associations attenuated by 35–75% in the fully adjusted models and remained significant for strain only [HR 1.3 (95% CI 1.0–1.7)], and the strain+ERI, ERI+injustice and strain+ERI+injustice combinations [HR 1.9 (95% CI 1.5–2.3), 1.6 (1.2–2.3) and 1.6 (1.3–2.0), respectively].
Clusters of aggregated work stressors and disability pension
Table 4 shows the risk of all-cause and cause-specific disability pension for the clusters of aggregated work stressors. In general, the results were in line with those obtained from self-reports, although with lower HR. Adjusted for demographics and region, all combinations of aggregated work stressors were associated with increased risk of all-cause disability pension while the stressors alone did not increase the risk. These risks attenuated by 35–46% after further adjustment for education and baseline mental and physical health and remained significant for the strain+ERI and strain+injustice combinations [HR 1.6 (95% CI 1.3–1.9) and 1.2 (1.0–1.4), respectively]. In relation to disability pension from depression, significant associations attenuated by 10–20% after full adjustments, showing a significantly increased risk for the ERI+injustice and strain+ERI+injustice combinations [HR 2.2 (95% CI 1.3–3.8) and 1.7 (1.1–2.7), respectively]. Regarding disability pension from musculoskeletal disorders, only the strain+ERI and ERI+injustice combinations adjusted for demographics and region associated with increased risk. After full adjustments, these associations attenuated by 52–59% and a significantly increased risk was observed for strain+ERI combination only [HR 1.5 (95% CI 1.2–1.9)]. Only one significant association of any single stressor with the study end-points was observed (between strain and disability pension due to depression), but even this lost its significance once fully adjusted.
Table 4
Combinations of aggregated work stressors and risk of disability pensiona. Finnish Public Sector Study employees eligible to the 2008 survey (N= 63 527) were followed until the end of 2011. Work-unit aggregates are based on survey responses from 3540 work-units. [CI=confidence interval; ERI=effort−reward imbalance; HR=hazard ratio.]
| Measurement, combination of stressors | Participants | Cause of disability pension | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Any cause (N= 1678) | Depression (N= 241) | Musculoskeletal (N= 814) | ||||||
|
|
|
|
||||||
| N | % | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Model 1b | ||||||||
| None | 32 287 | 50.8 | 1.00 | 1.00 | 1.00 | |||
| Strain only | 5437 | 8.6 | 1.24 | 0.96–1.59 | 1.38 | 1.04–1.83 | 1.26 | 0.90–1.76 |
| ERI only | 4753 | 7.5 | 1.15 | 0.79–1.68 | 1.26 | 0.89–1.78 | 0.96 | 0.61–1.50 |
| Injustice only | 7208 | 11.4 | 0.96 | 0.81–1.14 | 1.05 | 0.81–1.36 | 0.78 | 0.55–1.11 |
| Strain + ERI | 5172 | 8.1 | 2.06 | 1.65–2.57 | 1.45 | 1.02–2.06 | 2.17 | 1.60–2.95 |
| Strain + Injustice | 2701 | 4.3 | 1.33 | 1.04–1.70 | 1.14 | 0.88–1.48 | 1.46 | 1.05–2.04 |
| ERI + Injustice | 3392 | 5.3 | 1.41 | 1.06–1.88 | 2.40 | 1.35–4.27 | 1.23 | 0.95–1.60 |
| Strain + ERI + Injustice | 2577 | 4.1 | 1.38 | 1.07–1.78 | 1.78 | 1.09–2.92 | 1.01 | 0.66–1.54 |
| Model 2c | ||||||||
| None | 32 287 | 50.8 | 1.00 | 1.00 | 1.00 | |||
| Strain only | 5437 | 8.6 | 1.09 | 0.88–1.35 | 1.32 | 1.00–1.75 | 1.05 | 0.77–1.43 |
| ERI only | 4753 | 7.5 | 1.01 | 0.71–1.45 | 1.17 | 0.81–1.68 | 0.83 | 0.56–1.24 |
| Injustice only | 7208 | 11.4 | 0.98 | 0.87–1.12 | 1.02 | 0.79–1.31 | 0.83 | 0.62–1.10 |
| Strain + ERI | 5172 | 8.1 | 1.57 | 1.28–1.92 | 1.36 | 0.91–2.04 | 1.49 | 1.15–1.93 |
| Strain + Injustice | 2701 | 4.3 | 1.19 | 1.01–1.41 | 1.15 | 0.89–1.49 | 1.22 | 0.97–1.53 |
| ERI + Injustice | 3392 | 5.3 | 1.27 | 0.94–1.71 | 2.18 | 1.26–3.78 | 1.11 | 0.84–1.47 |
| Strain + ERI + Injustice | 2577 | 4.1 | 1.28 | 0.98–1.66 | 1.70 | 1.06–2.73 | 0.92 | 0.59–1.43 |
Discussion
This prospective cohort study of about 63 000 Finnish public sector employees with information on aggregated and 42 000 and self-reported job strain, ERI, and organisational injustice showed that these work stressors were clustered so that the observed prevalence of having no or several stressors was higher and having only one stressor lower than the expected prevalence. We found in the fully adjusted models that all combinations of self-reported and aggregated work stressors were associated with increased risk of disability pension compared to those free of job strain, ERI and injustice. In addition, self-reported strain and ERI alone were associated with increased risk of disability pension, although the strength of these associations was less than half of that observed for the work stressor clusters. More specifically, the combinations strain+ERI and strain+injustice were associated with the risk of all-cause disability pension while – in relation to cause-specific disability pensions – ERI+injustice and strain+ERI+injustice increased the risk of disability due to depressive disorders and strain+ERI disability due to musculoskeletal disorders. Increasing the credibility of our findings, these observations were obtained both from a register follow-up of a large cohort of eligible employees using objective aggregated measures of work stressors as well as a nested survey cohort using self-reported work data. We are not aware of previous studies on the clustering of work stressors and the risk of all-cause and cause-specific disability pension.
Most studies on work-related psychosocial factors are subject to subjectivity bias due to self-reported exposure measurements (4, 31) even though it has been argued that the effect of subjectivity on, for example, mean scores of ERI is not notable (32). Nevertheless, as, eg, sub-clinical depression may influence the reporting of working conditions and lead to disability pension during the follow-up, cohort studies that rely on self-reports of work stressors are open to reporting bias. Moreover, individual differences, such as tendency to experience negative emotions, may have an impact on how employees perceive and report work stress (21, 31, 33), and additionally affect their tendency to seek a disability pension. Reporting bias has been shown to inflate associations between job strain and the occurrence of depression (21). Use of work-unit-aggregated scores on the exposure is one way to control subjectivity and reporting biases (10, 11, 14, 21, 33), a method also used in the present study. However, as true between-individual differences within the unit of aggregation are lost when assigning the mean score for all members of a work unit, associations between work-unit aggregated work stressors and work disability are more likely to represent under- than overestimates (33). The strongest evidence comes from converging findings based on self-reports and the more conservative aggregated measures. The agreement of results based on aggregated and self-reported measures of work stressors suggest that response bias is an unlikely explanation to our findings on the association between work stress and risk of disability pension from any cause or depressive disorders.
Previous studies have suggested that the health influences of job strain, ERI, and organizational injustice are complementary (10, 18, 34–40). With few exceptions (18, 36, 37, 41, 42), a critical weakness in the prior evidence is, however, the reliance on cross-sectional designs (34, 35, 39, 40, 43) and the usage of only self-reported measures for both the exposure and the outcomes (34–36, 39, 41, 42). To the best of our knowledge, this is the only longitudinal study to examine clustering of work stressors and the risk of all-cause and cause-specific disability pension. Importantly, we were able to measure work stressors not only from self-reports but also independently based on work-unit aggregates (33). Moreover, the outcome was derived from reliable and accurate pension registers. Even though this study supports the suggestion that job strain and ERI are complementary (10, 18, 34–40), the measures of work stress also partly overlap. Job strain is considered to concern task-level imbalance between “efforts” and “rewards”, while ERI covers wider socioeconomic aspects, such as recognition and salary (44). ERI and organizational injustice (especially its distributive component, which was not included in present study) share similar conceptual background concerning the fairness of exchange. However, ERI is thought to operate on the individual level and in relation to rewards, while organizational injustice operates on the organizational level and in relation to other employees (36). Thus, an employee may find his/her efforts to be in balance with rewards but still find him/herself unequally treated when compared to other employees in the work unit.
We found that strain, ERI and organizational injustice are complementary to each other. The combination strain+ERI had a major impact on the risk of disability pension due to any cause or musculoskeletal disorders but a minor impact on the risk of disability pension due to depressive disorders. ERI+injustice had a minor impact on the risk of disability pension due to any cause or musculoskeletal disorders but a major impact on the risk of disability pension due to depression. We have previously found in a sample drawn from earlier phases of the FPS study that job strain was associated with increased risk of disability pension due to musculoskeletal diseases (11) while ERI was associated with disability pension due to depressive disorders (10). These present results highlight the importance of considering the work stressors combinations to better understand the risks they pose to employee health and work ability.
The plausible mechanism linking work stress and disability pension involve both physiological (ie, allostatic load) and emotional stress reactions, which may lead to health deterioration (16, 17). Allostatic load increases the risk of depression, diabetes mellitus and heart disease (16), may reduce blood flow to the muscles (which may cause nerve and tissue damage) and effectiveness of the immune system (causing impaired tissue reparation) (45). Stress response is additionally linked to various systemic risk factors, such as increased sterile inflammation, hyper-coagulation and cardiac arrhythmias, which can precipitate a serious vascular or cerebral event in vulnerable individuals (16, 17). Moreover, indirect effects of stress – like increased health risk behaviors (such as unhealthy diet, obesity, smoking, and sedentary lifestyle) (16, 33) – may worsen the symptoms of musculoskeletal diseases or limit an employee’s ability to recover from psychosocial and biomechanical workloads. Given that associations of different stressors with these multiple underlying mechanisms may slightly vary and the effects may accumulate, we hypothesized that multiple work stressors would be more harmful as risk factors for work disability than single stressors. There are various theoretical models to illustrate the effects of work stress. For example Lazarus et al (46) highlight the cognitive assessment of the stressful situation by the individual concerned. If the situation is perceived harmful, the possible coping strategies are then evaluated. Stress evolves individually in the course of time depending on the stressful situation, individual perceptions of it, and available coping strategies (46). Thus, it may be hypothesized that multiple stressors may have more harmful effects on employee health and work ability than single stressors because multiple stressors are likely to be perceived more stressful than a single ones. In this study, the observed prevalence of single stressors was smaller than expected suggesting that single stressors might not be perceived as harmful (or they may be more easily coped with) and thus less likely to be reported than multiple stressors. Lazarus and colleagues’ theory also points out the shortcomings of aggregated measures to assess work stress due to ignored true differences in perceived stress between individuals.
Limitations and strengths
There are some limitations to consider with this study. Even though we controlled for numerous baseline covariates, there is still a possibility of unmeasured confounding. Second, the response rate for study survey (71%) was reasonable. However, non-response may still have biased our results with self-assessed exposure, if stressed employees were more likely to respond than the non-stressed. Moreover, intra-class correlation coefficient (ICC) was low for aggregated ERI increasing possible misclassification bias and decreasing the ability to detect associations with study endpoints. Because ERI is a measure of individual expectations in terms of perceived fairness in gains received as compared to efforts made, it captures individual differences in addition to characteristics of the job and the work unit. A recently developed job exposure matrix for the assessment of psychosocial factors at work showed a good accuracy for job control and job strain, while its performance for other exposures was relatively low (47).
Strengths of this study include its prospective design and large study cohort, controlling for numerous confounding factors and supporting results with self-assessed and aggregated exposure. Moreover, the large cohort size enabled studying of risks related to various clusters of stressors. Furthermore, we used a reliable national pension register to assess the study endpoint (disability pension). In Finland, disability pension may be granted after approximately one year of sickness absence. Decisions are made based on a physician-written certificate with diagnosis according to ICD-10 and information on the treatment and rehabilitation received for the illness. The pension registers cover the entire Finnish population, which ensures practically no loss to follow-up.
Concluding remarks
We found that work stressors tend to cluster in the same individuals. The highest risk of disability pension was observed among those with strain+ERI, ERI+injustice or strain+ERI+injustice combinations, not among individuals with single stressors. In relation to disability pension due to depressive disorders, the combination of job strain+ERI+injustice and the combination of ERI+injustice were significant risk factors. In relation to disability pension due to musculoskeletal disorders, a significant risk factor was found to be the combination of strain+ERI. The results of this study show that instead of single stressors, it is important to study the clusters of work stressors, and that harmful combinations may vary depending on the health outcomes. These findings support the notion that improvement of work-related psychosocial factors may contribute to extensions to working life. To the best of our knowledge, no previous study has examined associations of multiple work stressors on disability pension or used more than one diagnosis-specific outcome.