Work patterns that differ from standard daytime hours, such as work in the evening or night as part of both rotating or permanent work patterns, have been associated with increased risk of injury (1–4). These work patterns are common, with 20% of employees in Denmark working schedules other than regular daytime shifts, of whom 8% work permanent night shifts (5). Among healthcare professionals in Denmark, 45% work patterns other than permanent dayshift, of whom 30% work night shift (5). The healthcare and social work sector has the highest number of occupational injury claims in Denmark (6). Injury, the physical harm as a consequence of an accident, both at work and outside of work is a leading cause of death among young adults in Denmark (7) and may result in disabilities (8, 9), lost work days (10) and poorer general health (11).
Sleepiness has been linked to reduced performance (12) and a higher risk of injury (12–14) and is suggested as a mechanism linking work patterns and risk of injury (15, 16). Employees working night shifts experience shorter and impaired sleep and poorer performance (17), which in turn may affect their alertness and decision-making abilities during work activities, as well as outside work (eg, impaired driving performance). This implies that night work and rotating work patterns may also affect the risk of injury outside work as sleepiness and poor performance carry over to commuting and leisure time.
Previous studies have found an increased risk of injury among individuals who work night compared to day shifts (18–20) or shifts other than the night shift (21, 22); similar results have been observed among workers with non-regular day work compared with those with regular day work (23, 24). Furthermore, the number of consecutive night shifts (4) and night shifts in the past week have been associated with a higher risk of injury (25, 26). However, few studies have been longitudinal (18, 19, 27) and most are based on self-reported, retrospectively collected information on work patterns (18, 22–24, 26, 27) and/or injury (18, 22–24, 26, 27), introducing possible bias due to non-participation, recall and reverse causality in cross-sectional designs. Furthermore, most previous studies have assessed the effects of evening or night work by comparing risk of injury among evening or night workers with day workers (18, 21–24, 26, 27). However, studies suggest that day, evening and night workers differ in terms of personality, lifestyle (28–30), as well as work tasks and work environment (29, 31, 32). Also, shift workers may be a highly selected group of people due to the “healthy worker effect” (29). These differences, which are unknown or rarely measured, may confound the association between work patterns and injury, as the group of exposed and the reference may not be exchangeable. Daily collection of working hours (eg, payroll data) provide a unique opportunity for longitudinal cohort studies with objective measures of the start and end times of work each day for each employee (33, 34). This daily information allows the same individual to contribute with risk time to both exposure and reference.
The purpose of this study was to (i) assess the association between working evening or night during the past seven days and risk of injury (occupational, transport and leisure time), compared to only day work during the past week; (ii) determine the association between the number of evening or night shifts worked during the past seven days and the risk of injury; and (iii) examine these associations when reducing unmeasured confounding in two restricted sub-populations of evening and night workers, respectively.
Methods
In this longitudinal study, we used a dynamic cohort of Danish hospital and administrative workers from 2007 to 2015. By use of the Danish personal identification number (35), work patterns were linked at the individual level to information on all injuries (occupational, commuting and leisure time injury) from national health and death registers. Daily information on exposure and injury allowed us to classify the number of evening or night shifts during the past week for each day at risk for each individual.
Total population
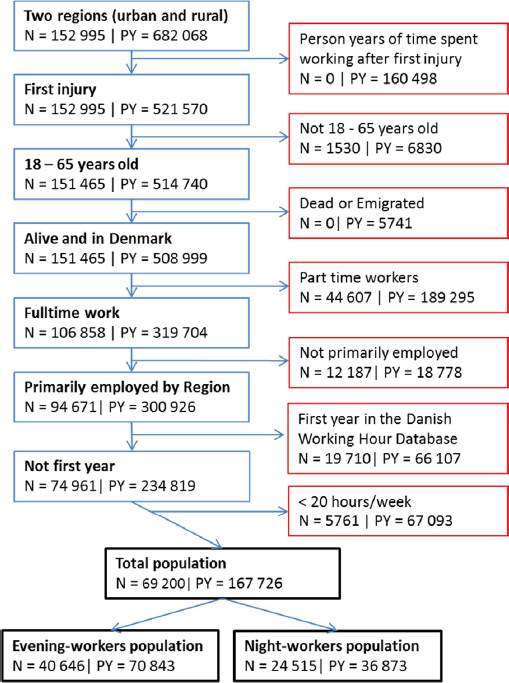
We included all employees in two regions of Denmark, covering urban and rural areas, registered with ≥1 shift during 2007–2015 (N=152 995). We excluded employees who were <18 or >65 years of age (N=1530), worked part-time (annual average <30 work hours/work week) (N=44 607), or worked <1 year according to the Danish Working Hour Database (DWHD) (N=19 710). The total population included 69 200 participants (see figure 1) with rotating or permanent day, evening and night workers.
Employees entered the study one year after their first registration in DWHD if they were primarily employed (eg, not self-employed or student) based on source for main income and 18 years old. They were followed until first injury, death, emigration from Denmark, 66 years of age, termination of employment or the end of follow-up, whichever came first. Participants were allowed to leave and re-enter the study population throughout follow-up. They were excluded temporarily (ie, did not contribute to risk time) when they were not primarily employed or worked <20 hours the previous week (eg, due to holiday, maternity leave and long-term sickness absence).
Sub-populations
To improve exchangeability between exposed and unexposed, two sub-populations of evening and night workers (with no permanent day, evening or night workers) were constructed. Based upon definitions by Härmä et al (36), the evening-worker population consisted of 40 646 employees with ≥12 days with evening shifts and ≥12 days with day shifts annually, evaluated monthly (figure 1). The night-worker population included 24 515 employees with ≥12 days with night shift and ≥12 days with day shifts annually (figure 1). Employees could contribute to both the evening- and night-worker population if they met both inclusion criteria.
Exposure assessment
Information on working hours was obtained from the DWHD, which includes payroll data, with exact time of start and end of each shift, primarily from all public hospital employees in Denmark from 2007–2015.
We defined three shifts based on the highest correlations in the study population between all actual clock hours at work: Day shift: ≥3 hours of work between 08:00–13:59 hours (rho: 0.83–0.99); evening shift: ≥3 hours of work between 16:00–21:59 hours (rho: 0.81–0.98); night shift: ≥3 hours of work between 00:00–05:59 hours (rho: 0.98–1.00).
For each calendar day, we evaluated if the employee had worked day, evening or night shifts during the past seven days. We then constructed four exposure variables related to the past seven days: evening work (yes/no), night work (yes/no), number of evening shifts (0–≥5 days with evening work), and number of night shifts (0–≥5 days with night work). Thus, employees could have both evening and night work in the same past week. On average the evening-worker population worked 38 evening shifts and 15 night shifts per person year while the night-worker population worked 41 evening shifts and 31 night shifts per person year.
Injury
Information on injuries was obtained from the National Patient Register (37) and the Danish Register of Causes of Death (38) and included both injuries at work and outside of work combined (ie, occupational, commuting and leisure-time injuries). The National Patient Register contains information on all patient contacts in both public and private Danish hospitals (37). We included all emergency room contacts with “accident” as the reason for the visit (39). All deaths of residents in Denmark are registered in the Danish Register of Causes of Death (38). We included all deaths with “accident” as cause of death or where the primary or supplementary cause of death was classified as ICD10 codes: S00-T79 and T90-T99 (injury, poisoning and certain other consequences of external causes), X00-X59, V01-W99 and Y10-Y34 (external causes of morbidity and mortality). For exact codes, see the study protocol (40).
Covariates
Information on covariates was derived from DWHD (age, sex, season, calendar year, previous sick leave, region and time since last shift) and Statistic Denmark’s Employment Classification Module (occupation and socioeconomic status, SES) (41). All included covariates were time-dependent by calendar day. Age was categorized as 18–24, 25–34, 35–44, 45–54 and 55–65 years. We classified SES as high (managers and high skilled jobs), intermediate (intermediate skilled jobs), and low (low or and unskilled jobs) (for exact codes see supplementary material, www.sjweh.fi/show_abstract.php?abstract_id=3737). Occupation was classified as administrative work (eg, secretaries, managers and scientific workers), jobs with patient contact (eg, doctors, nurses and porters) and technical staff (eg, technicians, chefs and cleaners), based on the Danish extended version of the classification of ISCO codes (41) with information on annual main source of income (see supplementary material). Previous sick leave (>10 days of sick leave within the previous year), weekly working hours (continuous), time since last shift [≤24, 25–72 and >72 hours from end of last shift till start of calendar day (00:00)], evening work in the past week (yes/no) and night work in the past week (yes/no) were based on DWHD. We used the first year of data for all employees to calculate baseline values for previous sick leave, evening workers, night workers as well as evening and night shifts.
Statistical method
We used Poisson regression to model incidence rate ratios (IRR) of injury as a function of evening or night work, with the log (person days) as offset. This reflects the time during which the response could occur (1), since injuries could happen over the entire day (both at and outside of work). Generalized estimating equations (GEE) with an independent correlation structure were used to account for repeated measures within employees. IRR with 95% confidence intervals (CI) were presented in three models. In model 1, estimates were adjusted for season and calendar year. Model 2 included model 1 and age, sex and occupation. Model 3 included model 2 and previous sick leave, weekly working hours, time since last shift, SES, region and – depending on the independent variable – night work in the past week in analyses of evening work or evening work in the past week in analyses of night work. Furthermore, we performed two sensitivity analyses based on model 2. In the first, weeks with night work were excluded from the analyses of evening work and, in the second, weeks with evening work were excluded from the analyses of night work. All analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC, USA) and performed on the total population as well as the two sub-populations of evening and night workers.
Results
Characteristics of the three populations are shown in table 1. In the total population, 167 726 person years (61 219 861 person days) and 11 834 first injuries were registered. The time-in-study ranged from 1–2830 days per employee, with a mean of 885 [standard deviation (SD) 757] days, and mean age at baseline was 40.5 (SD 11.2) years. Women, employees with patient contact, and employees with an intermediate SES contributed the majority of person years.
Table 1
Characteristics of the study population at baseline, cases and time in the study [PY=person years; SES=socioeconomic status].
| Total population a,b | Evening-workers population b | Night-workers population b | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| Baseline c N=69 200 | Cases N=11 834 | Person years d PY=167 726 | Baseline c N=40 646 | Cases N=5834 | Person years d PY= 70 843 | Baseline c N=24 515 | Cases N=3380 | Person years d PY=36 873 | |||||||
|
|
|
|
|
|
|
|
|
|
|||||||
| % | N | N | % | PY | % | N | N | % | PY | % | N | N | % | PY | |
| Age (years) | |||||||||||||||
| 18–24 | 5.4 | 3699 | 369 | 1.4 | 2392 | 5.1 | 2083 | 200 | 1.6 | 1162 | 5.6 | 1383 | 126 | 1.9 | 700 |
| 25–34 | 30.5 | 21 084 | 2863 | 18.0 | 30 187 | 34.1 | 13 840 | 1889 | 24.4 | 17 288 | 43.7 | 10 708 | 1458 | 34.7 | 12 804 |
| 35–44 | 26.0 | 17 989 | 3054 | 26.2 | 43 960 | 26.0 | 10 573 | 1535 | 27.8 | 19 659 | 24.9 | 6114 | 901 | 28.5 | 10 524 |
| 45–54 | 24.9 | 17 230 | 3223 | 31.9 | 53 453 | 23.9 | 9714 | 1411 | 29.7 | 21 027 | 18.8 | 4597 | 596 | 23.8 | 8761 |
| 55–65 | 13.3 | 9198 | 2325 | 22.5 | 37 734 | 10.9 | 4436 | 799 | 16.5 | 11 708 | 7.0 | 1713 | 299 | 11.1 | 4084 |
| Female gender | 75.6 | 52 292 | 8655 | 72.7 | 121 918 | 76.5 | 31 101 | 4349 | 73.7 | 52 228 | 76.4 | 18 723 | 2557 | 74.0 | 27 272 |
| Previous sick leave (>10 days) | 23.0 | 15 947 | 3144 | 21.3 | 35 793 | 23.9 | 9705 | 1608 | 23.0 | 16 278 | 22.8 | 5600 | 911 | 23.4 | 8624 |
| Occupation | |||||||||||||||
| Administration | 23.0 | 15 945 | 2244 | 25.1 | 42 075 | 12.7 | 5157 | 477 | 11.3 | 7997 | 3.7 | 897 | 74 | 2.8 | 1024 |
| Patient contact | 63.0 | 43 566 | 7603 | 61.1 | 10 2483 | 76.5 | 31 105 | 4710 | 78.8 | 55 837 | 90.9 | 22 279 | 3128 | 91.6 | 33 784 |
| Technical staff | 14.0 | 9689 | 1987 | 13.8 | 23 168 | 10.8 | 4384 | 647 | 9.9 | 7009 | 5.5 | 1339 | 178 | 5.6 | 2065 |
| SES | |||||||||||||||
| High | 28.3 | 19 586 | 3042 | 32.6 | 54 703 | 27.2 | 11 069 | 1412 | 29.2 | 20 710 | 31.1 | 7625 | 913 | 31.0 | 11 437 |
| Intermediate | 41.8 | 28 893 | 5362 | 44.7 | 75 036 | 49.4 | 20 061 | 3026 | 50.5 | 35 758 | 52.3 | 12 809 | 1925 | 53.5 | 19 732 |
| Low | 29.9 | 20 721 | 3430 | 22.7 | 37 987 | 23.4 | 9516 | 1396 | 20.3 | 14 375 | 16.7 | 4081 | 542 | 15.5 | 5704 |
| Danish region | |||||||||||||||
| Urban | 62.6 | 43 333 | 7475 | 63.9 | 107 086 | 62.5 | 25 412 | 3668 | 63.0 | 44 609 | 64.4 | 15 780 | 2261 | 64.7 | 23 870 |
| Rural | 37.4 | 25 867 | 4359 | 36.2 | 60 639 | 37.5 | 15 234 | 2166 | 37.0 | 26 235 | 35.6 | 8735 | 1119 | 35.3 | 13 003 |
The restricted population of evening workers included 40 646 employees, 5834 injuries and 70 843 person years. Compared with the total population, employees with patient contact or intermediate SES contributed a larger proportion of person years. The restricted population of night workers consisted of 24 515 employees resulting in 3380 cases and 36 873 person years. Compared with the total population at baseline, the night-worker population was younger [mean age 37.1 (SD 10.2) years] and a higher proportion had occupations with patient contact.
Table 2 shows the associations between injury and evening or night work in the total population, within evening as well as night workers. In the total population, employees had higher risk of injury after a week including evening work (IRR 1.32, 95% CI 1.26–1.37), and after a week including night work (IRR 1.33, 95% CI 1.25–1.41) compared with after a week with only day work, when adjusted for confounding (model 2).
Table 2
Evening and night work during the last week and IRR of injury in three models in the total population and two subpopulations [PY=person years; IRR=incidence rate ratio; CI=confidence interval].
| Cases | PY | Model 1 a | Model 2 b | Model 3 c | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||
| N | % (N) | IRR | 95% CI | P-value | IRR | 95% CI | P-value | IRR | 95% CI | P-value | |
| Total population | |||||||||||
| Evening work d1 | <0.001 | <0.001 | <0.001 | ||||||||
| Only day | 3195 | 22.1 (35 514) | 1 | 1 | 1 | ||||||
| Evening work | 7965 | 77.9 (125 020) | 1.41 | 1.35–1.47 | 1.32 | 1.26–1.37 | 1.23 | 1.17–1.29 | |||
| Number of evening shifts | <0.001 | <0.001 | <0.001 | ||||||||
| 0 | 8639 | 78.8 (132 212) | 1 | 1 | 1 | ||||||
| 1 | 1405 | 9.9 (16 540) | 1.33 | 1.26–1.41 | 1.25 | 1.18–1.32 | 1.22 | 1.15–1.30 | |||
| 2 | 880 | 5.7 (9624) | 1.43 | 1.33–1.53 | 1.32 | 1.23–1.42 | 1.23 | 1.14–1.32 | |||
| 3 | 504 | 3.1 (5249) | 1.50 | 1.37–1.64 | 1.40 | 1.28–1.53 | 1.25 | 1.14–1.37 | |||
| 4 | 235 | 1.5 (2447) | 1.50 | 1.32–1.71 | 1.41 | 1.24–1.60 | 1.23 | 1.07–1.40 | |||
| ≥5 | 171 | 0.9 (1654) | 1.61 | 1.38–1.88 | 1.54 | 1.32–1.80 | 1.28 | 1.09–1.49 | |||
| Test for trend: 1–≥5 shifts | 0.002 | <0.001 | 0.225 | ||||||||
| Night work d2 | <0.001 | <0.001 | <0.001 | ||||||||
| Only day | 1445 | 10.9 (15 362) | 1 | 1 | 1 | ||||||
| Night work | 7965 | 89.1 (125 020) | 1.47 | 1.39–1.56 | 1.33 | 1.25–1.41 | 1.21 | 1.12–1.32 | |||
| Number of night shifts | <0.001 | <0.001 | <0.001 | ||||||||
| 0 | 10 389 | 90.8 (152 363) | 1 | 1 | 1 | ||||||
| 1 | 691 | 4.2 (7099) | 1.53 | 1.41–1.65 | 1.38 | 1.28–1.50 | 1.37 | 1.22–1.53 | |||
| 2 | 389 | 2.5 (4214) | 1.44 | 1.30–1.60 | 1.27 | 1.15–1.41 | 1.20 | 1.06–1.35 | |||
| 3 | 201 | 1.4 (2328) | 1.35 | 1.17–1.55 | 1.20 | 1.04–1.38 | 1.08 | 0.93–1.25 | |||
| 4 | 97 | 0.6 (1016) | 1.49 | 1.22–1.81 | 1.37 | 1.12–1.67 | 1.19 | 0.97–1.46 | |||
| ≥5 | 67 | 0.4 (706) | 1.47 | 1.16–1.88 | 1.45 | 1.13–1.85 | 1.15 | 0.89–1.48 | |||
| Test for trend: 1–≥5 shifts | 0.339 | 0.876 | 0.294 | ||||||||
| Evening worker-population | |||||||||||
| Evening work d3 | <0.001 | <0.001 | <0.001 | ||||||||
| Only day | 2802 | 47.9 (31 252) | 1 | 1 | 1 | ||||||
| Evening work | 2479 | 52.1 (34 045) | 1.23 | 1.16–1.30 | 1.18 | 1.12–1.25 | 1.13 | 1.07–1.20 | |||
| Number of evening shifts | <0.001 | <0.001 | 0.004 | ||||||||
| 0 | 3032 | 55.9 (39 592) | 1 | 1 | 1 | ||||||
| 1 | 1303 | 21.8 (15 405) | 1.16 | 1.09–1.24 | 1.13 | 1.06–1.21 | 1.12 | 1.04–1.21 | |||
| 2 | 818 | 12.6 (8914) | 1.26 | 1.16–1.36 | 1.20 | 1.11–1.30 | 1.14 | 1.04–1.24 | |||
| 3 | 426 | 6.2 (4392) | 1.33 | 1.20–1.47 | 1.26 | 1.14–1.40 | 1.16 | 1.04–1.29 | |||
| 4 | 174 | 2.5 (1761) | 1.35 | 1.16–1.58 | 1.28 | 1.10–1.50 | 1.15 | 0.98–1.35 | |||
| ≥5 | 81 | 1.2 (779) | 1.42 | 1.14–1.77 | 1.37 | 1.10–1.71 | 1.17 | 0.94–1.47 | |||
| Test for trend: 1–≥5 shifts | 0.002 | 0.005 | 0.424 | ||||||||
| Night-worker population | |||||||||||
| Night work d4 | 0.003 | 0.021 | 0.498 | ||||||||
| Only day | 1219 | 50.5 (13 075) | 1 | ||||||||
| Night work | 1053 | 49.5 (12 814) | 1.13 | 1.04–1.23 | 1.10 | 1.01–1.20 | 1.04 | 0.93–1.15 | |||
| Number of night shifts | 0.089 | 0.214 | 0.521 | ||||||||
| 0 | 2161 | 64.5 (23 799) | 1 | 1 | 1 | ||||||
| 1 | 603 | 17.3 (6359) | 1.16 | 1.05–1.28 | 1.14 | 1.03–1.26 | 1.12 | 0.98–1.28 | |||
| 2 | 352 | 10.3 (3784) | 1.13 | 1.00–1.27 | 1.08 | 0.95–1.21 | 1.02 | 0.88–1.17 | |||
| 3 | 171 | 5.2 (1930) | 1.07 | 0.91–1.26 | 1.02 | 0.87–1.21 | 0.95 | 0.80–1.12 | |||
| 4 | 64 | 1.9 (698) | 1.11 | 0.86–1.43 | 1.09 | 0.84–1.40 | 1.00 | 0.78–1.30 | |||
| ≥5 | 29 | 0.8 (303) | 1.15 | 0.79–1.67 | 1.21 | 0.83–1.76 | 1.08 | 0.73–1.59 | |||
| Test for trend: 1–≥5 shifts | 0.508 | 0.522 | 0.256 | ||||||||
Similar, although attenuated estimates were observed for evening work in the past week among evening workers (IRR 1.18, 95% CI 1.12–1.25) and for night work among night workers (IRR 1.10, 95% CI 1.01–1.20).
In terms of number of evening and night shifts in the total population, a linear trend were found in the risk of injury across 1–≥5 evening shifts in the past week (P<0.001). The risk of injury was highest after one night shift during the past week (IRR 1.38, 95% CI 1.28–1.50) and lowest after three night shifts in the past week (IRR 1.20, 95% CI 1.04–1.38). Similar patterns were found for both 1–≥5 evening shifts in evening workers (linear trend: P=0.005) and 1–≥5 night shifts in the night workers (linear trend: P=0.522), though estimates were lower than in the total population.
The sensitivity analyses showed no major changes in estimates (evening work during the past week within evening workers: IRR 1.19, 95% CI 1.12–1.26, P<0.001; night work during the past week within night workers: IRR 1.10, 95% CI 0.99–1.22, P=0.084).
Discussion
In this large cohort study of hospital and administrative workers, a higher risk of injury was observed after evening and night work in the past week compared with only day work. Lower, but still elevated risks of injury after evening and night work persisted when we reduced group differences by restricting the population to evening and night workers, respectively. Risk of injury increased with more evening shifts in the past week. For night shifts, the risk of injury was lowest after three night shifts in the past week. Excluding days with night and evening work during the past week within analyses of evening and night work, respectively, did not change the conclusions.
With all workers included, our results of a higher risk of injury after evening and night work during the past week compared with day work, are generally in line with previous studies (19–22). Another study using payroll information found a higher risk of occupational injuries in afternoon shifts (IRR 1.66, 95% CI 1.23–2.25) and midnight shifts (IRR 1.72, 95% CI 1.26–2.36) compared with day shifts among US police officers (19). Where previous studies have mainly focused on occupational injuries (18, 19, 22–24), we analyzed all injuries. Our results on night work are consistent with a recent study among randomly selected Danish employees that used all injuries as the outcome [relative risk (RR) 1.11, 95% CI 1.06–1.17] (21).
A newly published systematic review found no linear risk of occupational injuries across number of consecutive afternoon/evening shifts based on three studies with only 2062 cases (4). Based on 5834 cases, we found an increasing risk of injury across the number of evening shifts in the past week. In model 3, no linear trend was observed. However, we suspect the model includes possible mediators and may be over adjusted.
We observed the lowest risk of injury after three night shifts in the past week, whereas previous cross-sectional studies have found a higher risk after three or more night shifts compared with none (25, 26). This deviation may be explained by a cruder categorization of night shifts and different confounding adjustment in previous studies. The present indication of a U-shaped risk could be a result of a combination of two different mechanisms. Sleepiness is most pronounced after the first and last (consecutive) night shifts (42), and thus the relative contribution of sleepiness is larger with few night shifts. On the other hand, sleep debt accumulates with increasing number of night shifts. Accordingly, sleepiness and therefore risk of injury is expected to be higher with more night shifts. When night work is unavoidable, our results indicate that three night shifts during the past week are preferable. However, more studies are needed to verify our results.
Most previous studies compare evening or night workers with day workers (18, 21–24, 26, 27). Even when results are adjusted for covariates, such as age, SES and weekly working hours, group differences between day, evening and night workers may still persist and lead to biased results. In our analysis of evening and night workers, employees could contribute with both exposed and unexposed risk time. This improved the exchangeability and reduced potential unmeasured confounding. The lower relative risk of injury following evening and night work within evening and night workers compared with the total population, suggests additional unmeasured confounding not accounted for by the confounding adjustment.
A previous, well-designed study, which also took group differences into account, found a higher risk of occupational injuries during afternoon shifts (RR 1.15, 95% Cl 1.07–1.23), and during night shifts (RR 1.23, 95% Cl 1.14–1.31) compared with morning shifts, when studying the shifts during which the injuries occurred (43). These findings are consistent with our results on evening work within evening workers and night work within night workers.
Strengths and limitations
The strengths of this study include the large study population, longitudinal design and the objective measures of both exposure and outcomes from reliable nationwide registers. This eliminates all recall bias. Detailed information from payroll data allowed us to calculate daily time-varying exposures thereby reducing misclassification. Moreover, by using a one year wash-out period prior to entry and only the first injury, we reduced the risk of reverse causation due to previous injuries, which may alter work patterns afterwards (44). All injuries (occupational, commuting and leisure time injuries) were included from national emergency room and death registers reducing the risk of bias from underreporting (45, 46). Lastly, little misclassification of timing of work in DWHD and shift categorizing is expected as these were based on actual shift schedules, largely covering definition from previous studies (19, 25, 34).
Unmeasured confounding was reduced by improving the exchangeability between exposed and unexposed. This may also reduce bias from self-selection into shift work. In addition, we adjusted for many potential confounders including season, sex and occupation. We also controlled for short job tenure and part-time work by excluding these from the study population. Working hours from multiple jobs within the regions were combined, but we had no information on jobs outside of the regions. However, by only including fulltime workers, we expect to have adjusted for most of the confounding from multiple jobs. Yet, task, workload, work environment, leisure-time activities, and traffic may be additional potential confounders if associated with shift patterns. Most of these differences are expected to decrease in the restricted populations, due to exclusion of, for example, daytime working administrative employees. Nonetheless, confounding from unmeasured individual differences may persist, since employees did not contribute with an equal amount of time to the exposure and reference groups and our results need to be confirmed in future studies. Furthermore, different characteristics of work patterns are highly correlated and the effects are therefore difficult to disentangle. Especially long shifts may have contributed to the higher risk of injury after evening work during the past week. Moreover, rest breaks, on-call shifts, quick-returns and rotating work may be of interest to consider in future studies.
No information on exact time of the injury was available, thus there is a risk of assessing work patterns after the injury. However, injuries are only admitted to emergency rooms in Denmark within 24 hours after occurrence. By assessing the exposures up until the day before the injury the risk of reverse causation was reduced.
The populations of evening and night workers did not include permanent evening or night workers. Whether risks are similar in permanent evening and night workers remains to be settled. Thus, the results are generalizable to workers with some day work in Denmark and should be interpreted with caution in other countries and with respect to job groups with similar work patterns. Furthermore, we expect the mechanisms to be similar for minor injuries.
In conclusion, we find an increased risk of injury after evening and night work among Danish hospital employees compared with day work during the past week. The higher risks persist, though attenuated, when unmeasured confounding from differences between day, evening and night workers was reduced. While a dose–response for number of evening shifts was found, in our study, three night shifts during the past week seem to be preferable in relation to risk of injury.