Mental health problems are prevalent in the working-age population of many developed countries (1). Important consequences are high rates of sickness absence and unemployment, resulting in enormous societal costs (1) and individual suffering (2, 3). Common mental health problems are mild-to-moderate depressive, anxiety, and stress-related complaints, which have also been described as common mental disorders (CMD) (1). The large impact of CMD on society has led to a growing attention in recent literature for the development and evaluation of interventions that aim to promote return-to-work (RTW) of workers on sick leave due to a CMD (4–14). Many of these studies focused on sick-listed employees, ie, workers with an employment contract.
Up to now, little attention has been paid to the development and evaluation of RTW interventions for sick-listed workers without an employment contract, such as temporary agency workers, those with an expired fixed-term contract, and unemployed workers (15). This is an important concern as these workers seem to have a more vulnerable position in the labor market. Compared to sick-listed employees, they appear to be at risk of longer disability episodes (16, 17). Moreover, in the last decennia, flexible forms of employment – such as temporary employment – have globally expanded (18, 19).
In the Netherlands, sick-listed workers without an employment contract are entitled to sickness benefit payment and occupational healthcare (OHC) by the Dutch Social Security Agency (SSA). Within this group, mental health problems are the most common reason for sick-listing (20, 21). Often these workers experience several (psychosocial) RTW barriers and have a negative perception of their health condition (22). In many cases, the absence of a workplace to return to is the main RTW obstacle (23).
A participatory, supportive RTW program was developed to promote RTW of workers who filed a sickness benefit claim at the Dutch SSA due to a CMD. The program was based on an existing participatory approach, which had previously shown promising results among a similar group of workers sick-listed due to musculoskeletal disorders (24). Direct placement in a competitive job by a vocational rehabilitation agency was added to the program to overcome the main RTW obstacle, ie, the absence of a workplace. Moreover, through application of an integrated care approach, collaboration between OHC professionals of the Dutch SSA and (mental) healthcare providers was stimulated within this new program.
In this study, we present the effects of the participatory, supportive RTW program. The main aim of this study was to evaluate the program’s effectiveness in reducing the duration until first sustainable RTW in competitive employment, compared to usual OHC by the Dutch SSA. Secondary outcome measures were average working hours, duration until RTW in any type of employment, sickness benefit duration, and perceived physical and mental health and functioning.
Methods
Study design and setting
The study design consisted of a randomized controlled trial (RCT) with two arms – an intervention and control group – and a follow-up period of 12 months. Entitled the “Co-WORK study”, this trial was conducted in collaboration with seven offices of the Dutch SSA, located in three districts, and three vocational rehabilitation agencies. The Medical Ethics Committee of the VU University Medical Center approved the study design and all participants signed informed consent. The trial was registered at the Dutch Trial Register (Nederlands Trial Register) (NTR3563).
Study population and recruitment
Sick-listed workers (18–64 years), who applied for a sickness benefit at the Dutch SSA due to the (partial) absence of an employment contract and belonged to one of the participating SSA offices, received an invitational letter together with a short questionnaire 1–2 weeks after being sick-listed. Because during recruitment it was no longer possible to recruit on the basis of a registered mental health complaint, every newly sick-listed worker received an invitation and was asked to indicate whether he/she was sick-listed due to mental health problems. Furthermore, the short questionnaire consisted of a screener for distress (25), questions about the intention to return to work despite ongoing health complaints, and about the date of sick-listing. The RTW intention was measured on a 5-point Likert scale with responses: “certainly not”, “probably not”, “maybe”, “probably”, and “certainly”. Sick-listed workers could only participate if they experienced an elevated level of distress and were sick-listed for ≤14 weeks. Exclusion criteria included: (i) not being able to complete questionnaires written in the Dutch language; (ii) having a conflict with the SSA regarding a sickness benefit claim or a long-term disability claim; (iii) the presence of a legal conflict, eg, an ongoing injury compensation claim; (iv) a sickness absence episode due to a CMD within one month before the current sickness benefit claim; (v) already having received usual OHC since the start of the current sickness absence period; (vi) pregnancy, up until three months after delivery; (vii) no signed informed consent form; and (viii) probably/certainly not having the intention to return to work despite ongoing health complaints. This latter criterion was based on findings of two earlier studies (12, 24), which showed that sick-listed workers without this positive RTW intention require another type of intervention (12). Sick-listed workers who were willing to participate and met the criteria for eligibility, were contacted by the researcher by telephone to screen for other in- and exclusion criteria.
After randomization, intervention group participants could still be excluded from participation in the RTW program in case their insurance physician assessed a (medical) contraindication for participation. However, these individuals remained in the intervention group, based on the intention-to-treat principle.
Randomization and blinding
Randomization was performed at participant level. To ensure an equal distribution, prestratification was applied to different types of workers (before sick-listing) – ie, unemployed, temporary agency, and fixed-term contract worker – and the three participating SSA districts. A block randomization table with a fixed block size of four was generated for each stratum, based on schemes with random permuted numbers. Randomization was performed by a research assistant during an intake meeting with the participant.
Blinding participants and professionals for the randomization result was not possible due to the nature of the intervention. To minimize bias caused by self-report, we collected registered data from the SSA when possible. A research assistant entered all data into a database using a unique research number for each participant to guarantee blinded analyses by the researcher.
Interventions
Dutch SSA usual care
The Dutch SSA provides OHC in a team of professionals, consisting of a RTW coordinator, an insurance physician and a labor expert. The RTW coordinator investigates why the sick-listed worker thinks that he/she is unable to work. He/she monitors the full vocational rehabilitation process and refers the worker to the insurance physician or labor expert if necessary. The insurance physician is encouraged to follow the guidelines for OHC of the Dutch Society of Occupational Medicine. He/she advises the sick-listed worker about recovery and RTW based on a medical problem analysis. If necessary, he/she refers to further treatment options to prevent work disability. The labor expert provides vocational rehabilitation support and advises the sick-listed worker about RTW options, using his/her expertise of the labor market. He/she can decide to refer the sick-listed worker for additional support, such as assistance from a vocational rehabilitation agency.
The RTW program
Participants of both groups received usual OHC from the SSA. However, participants in the intervention group were referred to a more standardized form of OHC that started early after sick-listing, ie, the participatory supportive RTW program.
Within two weeks after allocation of the participant to the program, the RTW coordinator conducts an analysis followed by a medical problem analysis by the insurance physician. Subsequently, the latter contacts the participant’s healthcare provider(s) to agree on treatment and RTW. The RTW coordinator encourages the participant to play an active role in his/her own vocational rehabilitation process and to list all RTW obstacles. This list is then used as a starting point for a meeting between the worker and the labor expert, in which all obstacles are jointly prioritized. Also the RTW coordinator, with help from the labor expert, makes a list of RTW obstacles facing this particular worker. Subsequently, in the following two weeks, the participant has another meeting with both the RTW coordinator and the labor expert, during which they jointly search for solutions to overcome the prioritized obstacles and discuss suitable work. When consensus is reached, solutions and suggestions to find suitable work are summarized in a RTW action plan. During the making of this action plan, the participant’s responsibility in implementing the action plan is emphasized. To facilitate the job search, the participant is referred to a vocational rehabilitation agency. Within another four weeks, this agency offers the participant ≥2 competitive jobs with a minimum contract period of three months, matching with the RTW action plan. The RTW coordinator monitors the process and refers the participant to another vocational rehabilitation agency for additional support if necessary.
More information about the study design and setting, procedures used for recruitment, randomization and blinding, the sample size calculation, and the participatory, supportive RTW program can be found in the study protocol (26).
Assessment of protocol adherence and contamination
We used findings of our previous process evaluation to assess the number of intervention group participants that participated in each step of the program. These findings have been described in more detail elsewhere (27). For all participants, we assessed both registered information about consultations with SSA professionals and self-reported information about additional vocational rehabilitation support or medical cointerventions.
Outcome measures and data collection
Data regarding paid employment, sickness absence, and type of worker were collected from the SSA database. Additional data on RTW and sickness absence were assessed every three months using questionnaires. Other outcomes were measured every six months. Possible confounders were measured at baseline, after informed consent was signed and prior to randomization.
Primary outcome measure
The primary outcome was the duration in calendar days from the day of enrollment in the study until first paid employment in a regular work-setting for ≥28 consecutive calendar days. It was possible that the participant was still partially at work at the time of enrollment in the study. In that case, the participant was considered to have reached the outcome if he/she had returned to work for the hours for which he/she had been sick-listed. Our RTW assessment was not restricted to full work resumption. The first and third authors assessed this outcome while the second author checked this interpretation on inconsistencies in ten random cases.
Secondary outcome measures
To assess the average working hours per week, we divided the total working hours by the total number of weeks in competitive employment during follow-up.
To measure the duration until first employment in any type of work, both RTW in paid and unpaid labor were included, regardless of the duration of the work resumption.
In line with Vermeulen et al (24), the sickness benefit period was defined as the duration between the day of enrollment in the study until ending of this benefit for ≥28 days.
The Four-Dimensional Symptom Questionnaire (4DSQ) (28) and the Dutch translation of the 36-item Short Form Health Survey (SF-36) (29) were used to assess perceived mental and physical health and functioning. The 4DSQ consists of four scales measuring perceived symptoms of distress, anxiety, depression and somatization (28). The SF-36 consists of eight scales: physical functioning, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health. These scales were used to construct two summary component scores (physical and mental) for our population relative to standard scores, with a standard mean of 50 (29, 30).
Possible confounders
Earlier studies found associations between RTW or sickness absence duration of sick-listed workers with mental health problems and their age (16,31,32), type of worker (16, 32), RTW expectations (31), and RTW intention (12, 24). Therefore, information was gathered about these possible confounders. We also assessed other demographic characteristics, ie, gender and education. To assess type of worker, we examined type of worker before sick-listing, the presence of an employment contract at baseline, the work schedule in the participant’s last job, the average number of working hours a week, and the years worked in this kind of employment.
The participant’s expectations of being able to fully return to work in the next six months were assessed on a 5-point Likert response scale and dichotomized into “very sure/sure” or “not sure nor unsure/unsure/very unsure”.
RTW intention and underlying behavioral determinants, ie, Attitude, experienced Social influence and self-Efficacy regarding RTW (ASE), were assessed with a questionnaire developed earlier by Van Oostrom et al (12, 33). The same item used earlier in the screening questionnaire was used again to assess the RTW intention despite ongoing health complaints. In addition, the relation between health complaints and work resumption was assessed with the fear avoidance beliefs subscale of the Dutch Work Reintegration Questionnaire (WRQ) (34, 35).
Statistical analyses
When multiple-scale questionnaires were used, first sum scores were computed for each scale. In case of missing items, the average score of the items in the same scale were imputed for the missing items, but only in cases where at least half of the items in this scale were valid.
Descriptive statistics were used to compare baseline characteristics of the intervention and control groups. T-tests for continues variables and Pearson Chi-Square tests for categorical variables were performed to assess the statistical significance of possible differences between groups.
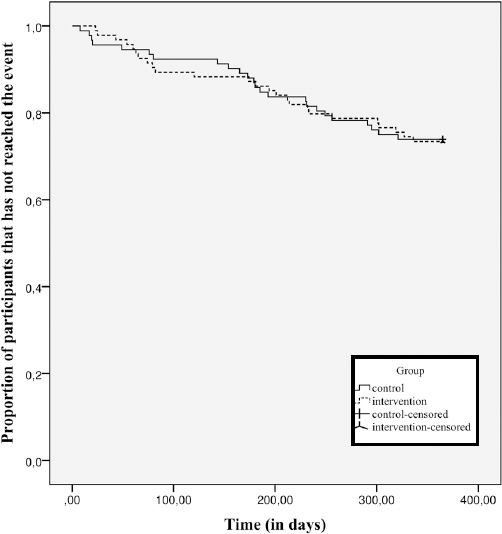
Techniques originating from survival analysis were used to analyze the effects of allocation to the intervention or control group on duration until first sustainable RTW in a competitive job, duration until RTW in any type of work, and the sickness benefit duration. Kaplan Meier curves were plotted to describe the duration until these outcomes in both groups. When no median duration could be assessed because <50% of the participants eventually reached the outcome, we instead assessed the duration until the outcome was reached by ≥25% of the participants. Subsequently, Cox regression analysis was used to estimate the hazard ratio’s (HR) for these outcomes and corresponding 95% confidence intervals (CI). In case the proportion between the Kaplan Meier curves seemed to change over time, we investigated whether the HR were significantly different for different time periods by adding an interaction term between group and a time dependent covariate to the model.
Linear regression analyses were applied to investigate differences between the two groups in the average working hours per week.
Linear mixed models were used to investigate the longitudinal effect on perceived mental and physical health and functioning. The models were adjusted for differences in outcomes at baseline. To adjust for the dependency of multiple measurements in time within the same participant, a random intercept was included. We also accounted for possible clustering at the level of participating SSA offices. Random coefficients were added to the model at this level in case the difference between the results of the -2 log (restricted) likelihood tests of the new and previous model differed at least 3.84 points, after adding a random intercept, and 5.99 points, after adding a random slope.
All analyses were adjusted block-wise for possible confounding factors. The analyses were applied according to the intention-to-treat principle. In addition, per-protocol analyses were performed. For all analyses a P-value of <0.05 (two-tailed) was considered statistically significant. The analyses were performed in SPSS 22 (IBM, Armonk, NY, USA).
Results
Participant flow
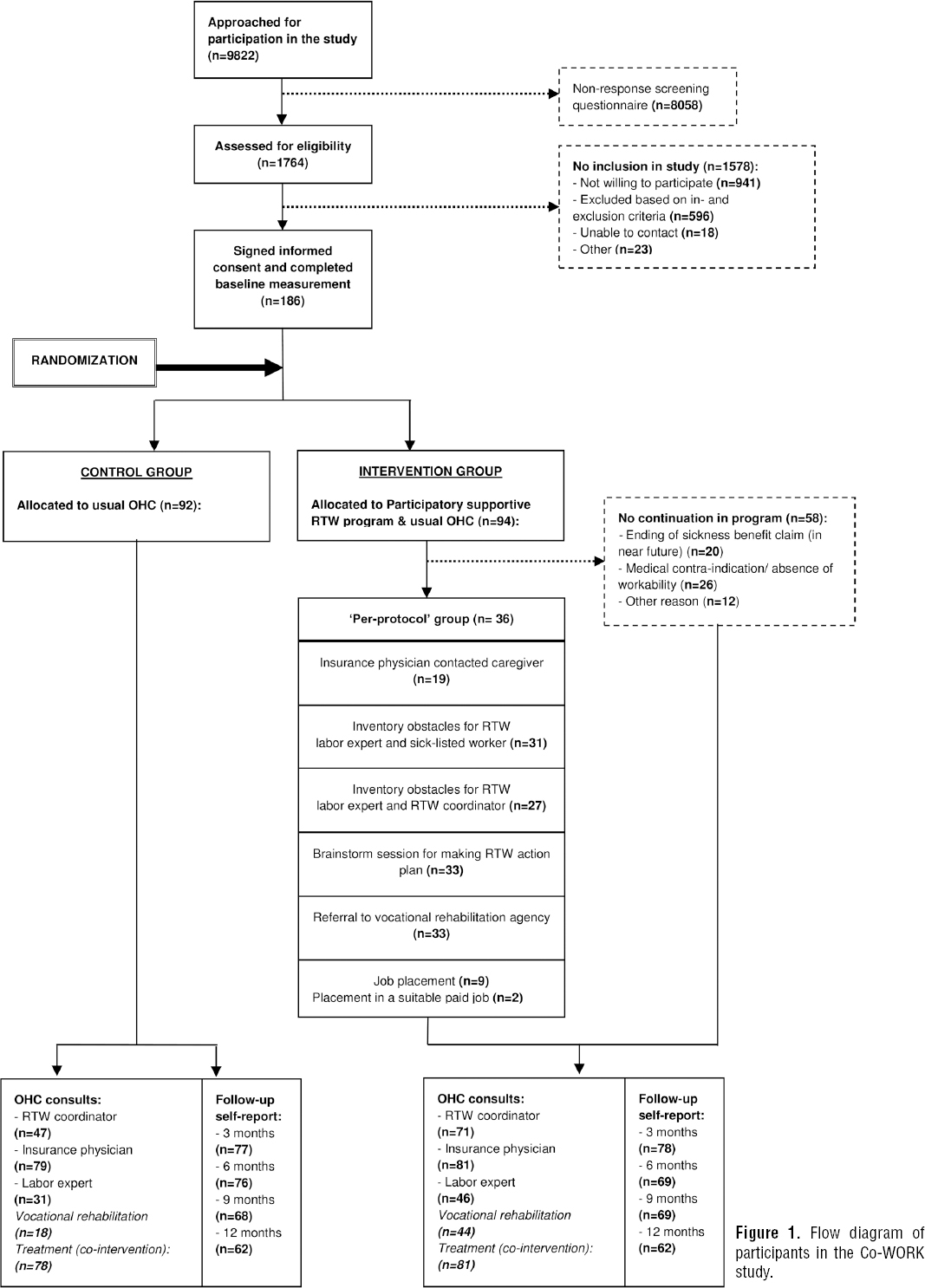
The flow of sick-listed workers in the Co-WORK study is illustrated in figure 1. Between March 2013 and September 2014, 9822 sick-listed workers were approached for participation in the study. In total, 186 participants were included in the study and randomly allocated to an intervention (N=94) or control (N=92) group.
Loss to follow-up
Data about paid employment, sickness absence, type of worker, and SSA consultations could be collected from the SSA database for all participants (100%). Availability of self-reported data within each group is illustrated in figure 1.
Baseline characteristics
Table 1 presents the baseline characteristics of participants in both groups. There were mainly small, non-significant differences between the groups, except for the expectation regarding RTW within six months (P<0.01).
Table 1
Baseline characteristics. [ASE=attitude experienced social influence and self-efficacy regarding return to work (RTW); SF-36=36-item short form health survey; SD=standard deviation; 4DSQ=4-dimensional symptom questionnaire.]
| Variable | Intervention group (N=94) | Control group (N=92) | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| N | % | Mean | SD | N | % | Mean | SD | |
| Gender (female) | 45 | 48 | 47 | 51 | ||||
| Age (years) | 45.7 | 10.6 | 46.3 | 10.0 | ||||
| Education (low) a | 26 | 28 | 23 | 25 | ||||
| Type of worker | ||||||||
| Type of worker before reporting sick | ||||||||
| Unemployed | 88 | 94 | 85 | 92 | ||||
| Temporary agency | 4 | 4 | 2 | 2 | ||||
| Fixed-term contract | 2 | 2 | 5 | 5 | ||||
| Employment contract at baseline (yes) | 11 | 12 | 14 | 15 | ||||
| Work schedule in last job, day work | 72 | 77 | 75 | 82 | ||||
| Working hours per week in last job b | 32.6 | 11.6 | 31.4 | 10.8 | ||||
| Years worked in last job c | 10.0 | 10.0 | 8.7 | 9.6 | ||||
| Expectation regarding ability for full RTW in 6 months, (very) certain | 4 | 4 | 16 | 17 | ||||
| ASE questionnaire d | ||||||||
| Intention to RTW (yes) | 78 | 83 | 81 | 88 | ||||
| Attitude (6–30 score) | 15.7 | 5.2 | 14.9 | 4.2 | ||||
| Normative beliefs (4–20 score) | 12.0 | 3.1 | 12.6 | 2.6 | ||||
| Social modeling (2–10 score) | 4.8 | 1.9 | 4.8 | 1.5 | ||||
| Self-efficacy (2–10 score) | 6.3 | 1.8 | 6.2 | 1.6 | ||||
| Fear avoidance beliefs (4–40 score) e | 29.0 | 6.9 | 28.5 | 7.0 | ||||
| 4DSQ f | ||||||||
| Distress (0–32 score) | 25.8 | 5.1 | 26.3 | 5.4 | ||||
| Depression (0–12 score) | 6.7 | 3.7 | 6.8 | 3.9 | ||||
| Anxiety (0–24 score) | 10.7 | 6.1 | 9.8 | 6.7 | ||||
| Somatization (0–32 score) | 14.9 | 5.9 | 15.5 | 7.2 | ||||
| SF-36 g(component summary score) | ||||||||
| Physical | 46.4 | 9.5 | 47.7 | 9.3 | ||||
| Mental | 21.0 | 8.5 | 22.1 | 9.1 | ||||
d A lower score on these scales corresponds with a more positive attitude regarding RTW (attitude), the belief that other people think work resumption is important (normative beliefs), finding it more important what other people think (social modelling) and a stronger feeling of self-efficacy regarding RTW (self-efficacy).
Occupational healthcare
Figure 1 illustrates the OHC during follow-up in both groups. Only 36 intervention group participants (38%) continued with the program after the medical problem analysis. These participants are referred to as the “per-protocol group”. In case of a medical contraindication (N=26), the participant continued in usual OHC instead. Participants whose sickness benefit had already ended or was likely to end early after randomization because recovery of workability was established (N=20), were by law (soon) no longer entitled to OHC by the SSA, and as such could no longer participate in the program.
Figure 1 shows how many of the per-protocol participants (N=36) participated in each step of the program. The figure also shows the number of participants in the intervention and control groups that had ≥1 consultations with an SSA professional as well as information about referral to a vocational rehabilitation agency and medical cointerventions.
Primary outcome measure
In the intervention and control groups, 25 (27%) and 24 (26%) participants, respectively, returned to work sustainably during follow-up. After 327 days in the intervention group and 302 days in the control group, ≥25% of the participants had returned to work sustainably. The range between the minimum and maximum duration until this outcome in the intervention and control group was respectively 23–336 days and 8–321 days. Figure 2 illustrates the unadjusted Kaplan Meier curves for time until first sustainable RTW in the two groups. Table 2 presents the crude and adjusted HR. In none of the models a significant effect of allocation to the intervention compared to the control group was found. Also the per-protocol analysis showed no significant effect.
Table 2
Results of the Cox regression analyses. Reference group is the control group in all models. [95% CI=95% confidence interval; RTW=return to work.]
| HR a | 95% CI | P-value | HRb | 95% CI | P-value | HR c | 95% CI | P-value | HR d | 95% CI | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time to first sustainable RTW in competitive employment | 1.02 | 0.58–1.78 | 0.95 | 1.00 | 0.57–1.75 | 0.99 | 0.98 | 0.55–1.77 | 0.96 | 1.15 | 0.61–2.16 | 0.67 |
| Time to first RTW in any type of employment | 0.88 | 0.56–1.37 | 0.56 | 0.87 | 0.56–1.36 | 0.54 | 0.92 | 0.57–1.47 | 0.72 | 0.99 | 0.58–1.67 | 0.96 |
| Sickness benefit duration (days) | ||||||||||||
| ≤240 | 0.75 | 0.47–1.19 | 0.22 | 0.76 | 0.47–1.21 | 0.24 | 0.75 | 0.46–1.22 | 0.25 | 0.74 | 0.45–1.23 | 0.24 |
| >240 | 2.19 | 0.84–5.70 | 0.11 | 2.11 | 0.81–5.51 | 0.13 | 2.16 | 0.82–5.70 | 0.12 | 2.27 | 0.85–6.07 | 0.10 |
Secondary outcome measures
Working hours per week
Participants in the intervention and control groups who were employed during follow-up worked on average respectively 26.3 [standard deviation (SD) 12.6] and 25.6 (SD 14.1) hours per week, which did not differ significantly (adjusted B -0.62, 95% CI -10.83–9.59, P=0.90). Also the per-protocol analysis revealed no significant differences between groups.
RTW in any type of employment
In total, 37 intervention group participants (39%) and 40 control group participants (43%) returned to work in paid or unpaid labor. After 181 and 167 days, ≥25% of the participants in the intervention and control groups, respectively, had reached this outcome. The range in duration until this outcome was 14–342 days in the intervention group and 8–348 days in the control group. Both the crude and adjusted HR are presented in table 2. Significant effect of allocation to the intervention compared to the control group was found neither in these models nor the per-protocol analysis.
Sickness benefit period
The sickness benefit ended for 45 (48%) and 47 (51%) participants in the intervention and control groups, respectively. After 89 days, the sickness benefit had ended for ≥25% of the participants in both groups, with a range of 8–336 days in the intervention group and 14–329 days in the control group. The HR for the intervention compared to control group were found to differ significantly (P<0.05) before and after 240 days. Table 2 presents the crude and adjusted HR for both periods and shows no significant differences between groups. Results of the per-protocol analysis differed slightly. This analysis revealed a significant delayed ending of the sickness benefit in the first 240 days for the per-protocol group in comparison with the control group (adjusted HR 0.30, 95% CI 0.12–0.75, P=0.01), followed by a non-significant trend towards an earlier ending of the sickness benefit in this first group after 240 days (adjusted HR 2.79, 95% CI 0.95–8.15, P=0.06).
Health related outcomes
Table 3 summarizes the results of the (adjusted) mixed-model analyses. We found no significant differences in health outcomes between the two groups. The per-protocol analyses also revealed no significant differences between the per-protocol and control group.
Table 3
Results of the mixed model analyses. [95% CI=95% confidence interval; 4DSQ=4-dimensional symptom questionnaire; SD=standard deviation; SF-36=36-item short form health survey.]
| Outcomes | Average intervention effect during follow-up | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| 6 months | 12 months | |||||||||||||||
|
|
|
|
||||||||||||||
| Mean | SD | Mean | SD | ß a | 95% CI | P | ß b | 95% CI | P | ß c | 95% CI | P | ß d | 95% CI | P | |
| 4DSQ e | ||||||||||||||||
| Distress (0–32 score) | ||||||||||||||||
| Intervention | 19.1 | 8.4 | 17.5 | 10.1 | -0.27 | -2.54–2.01 | 0.82 | -0.13 | -2.37–2.10 | 0.91 | 0.20 | -2.11–2.50 | 0.87 | -0.10 | -2.52–2.32 | 0.94 |
| Control | 20.1 | 8.7 | 17.9 | 10.0 | ||||||||||||
| Depression (0–12 score) | ||||||||||||||||
| Intervention | 4.5 | 4.1 | 3.7 | 4.3 | -0.10 | -1.02–0.82 | 0.84 | 0.04 | -0.95–0.86 | 0.92 | -0.01 | -0.94–0.92 | 0.98 | 0.0 | -0.98–0.98 | 1.0 |
| Control | 4.5 | 4.0 | 4.6 | 4.2 | ||||||||||||
| Anxiety (0–24 score) | ||||||||||||||||
| Intervention | 6.7 | 5.8 | 6.1 | 6.3 | -0.88 | -2.27–0.51 | 0.21 | -0.83 | -2.23–0.57 | 0.24 | -0.92 | -2.36–0.53 | 0.21 | -1.05 | -2.58–0.49 | 0.18 |
| Control | 7.8 | 6.8 | 6.9 | 7.4 | ||||||||||||
| Somatization (0–32 score) | ||||||||||||||||
| Intervention | 12.5 | 7.2 | 12.1 | 7.6 | 0.28 | -1.37–1.93 | 0.74 | 0.35 | -1.30–2.0 | 0.68 | 0.59 | -1.11–2.29 | 0.49 | -0.09 | -1.86–1.69 | 0.92 |
| Control | 12.8 | 7.2 | 11.4 | 8.0 | ||||||||||||
| SF-36 f | ||||||||||||||||
| Physical component | ||||||||||||||||
| Intervention | 47.8 | 10.1 | 46.1 | 10.4 | -0.19 | -2.39–2.01 | 0.87 | -0.45 | -2.55–1.65 | 0.67 | -0.47 | -2.61–1.68 | 0.67 | -0.69 | -2.96–1.58 | 0.55 |
| Control | 47.7 | 9.0 | 48.3 | 10.6 | ||||||||||||
| Mental component | ||||||||||||||||
| Intervention | 31.5 | 11.6 | 35.5 | 12.8 | 1.31 | -1.93–4.54 | 0.43 | 1.12 | -2.08–4.32 | 0.49 | 0.89 | -2.35–4.13 | 0.59 | 1.59 | -1.83–5.01 | 0.36 |
| Control | 31.5 | 12.3 | 32.8 | 13.6 | ||||||||||||
Discussion
Main findings
The present study showed no significant superior or adverse effect of allocation to the participatory, supportive RTW program on the duration until first sustainable RTW in comparison with usual OHC by the Dutch SSA. Furthermore, no significant differences were found in favor of the intervention group on any secondary outcome.
Interpretation of findings
The absence of an intervention effect on the duration until sustainable RTW could be explained by implementation failure. A very low number of intervention group participants actually participated in the RTW program (N=36), and even in this per-protocol group, protocol adherence was only low to moderate (27). We tried to enhance protocol adherence by a detailed protocol description and organizing follow-up training sessions for participating professionals. Still, the main stakeholders in our study experienced several barriers to the program’s successful execution (36).
Some aspects of this implementation failure also played a role in the evaluation of other RTW programs, which reveals that improving OHC in daily practice is difficult. For example, a recent Dutch study by Audhoe et al (37) evaluating a new RTW program aimed at a comparable population, ie, non-permanent workers with psychological problems, also revealed low protocol adherence by Dutch SSA professionals and unsuccessful counseling by contracted vocational rehabilitation agencies. Their explanations for this low protocol adherence were similar to the barriers mentioned by the stakeholders in our study, namely, organizational constraints and limited availability of suitable workplaces (36, 37). Furthermore, in a recent study about an integrated workplace intervention for Dutch workers with rheumatoid arthritis, Van Vilsteren et al (38) found that it was difficult to implement an integrated care approach. This is in line with an earlier Dutch study by Anema et al (39) that revealed limited collaboration between OHC professionals and other healthcare providers in the Netherlands.
An important consequence of the implementation failure in our study was less continuity in OHC than was prescribed in the protocol. Because continuity in OHC is considered important in enhancing RTW (40, 41), this may have influenced the effectiveness of the new program. This means that it remains unclear what the results would have been if the program had been executed according to protocol.
Nevertheless, comparing the effectiveness of a participatory RTW program across studies reveals more promising results for sick-listed workers with physical complaints compared to those with mental health problems. To illustrate, in Canada and the Netherlands, beneficial effects of a participatory RTW program on work-related outcomes were found for sick-listed employees with low back pain (42–44) and on the duration until sustainable RTW of workers without an employment contract and sick-listed due to musculoskeletal disorders (24). Whereas, in line with our findings, no superior (overall) intervention effect on the duration until sustainable RTW was found for Dutch sick-listed employees with a CMD (12), and an adverse effect of a very similar program was found for Danish sickness absence beneficiaries with mental health problems (7). Furthermore, although we selected participants with positive RTW intentions and our analyses were adjusted for possible changes in this intention, findings were inconsistent with the beneficial intervention effect found for a similar subgroup of employees sick-listed due to a CMD with such positive intention at baseline (12). This suggests a discrepancy in findings for sick-listed workers with a CMD who still have an employment contract and those who no longer have an employment contract.
Although implementation failure will have played a role in the discrepancy in findings between our and the aforementioned studies, this discrepancy may also suggest that our RTW program has not properly addressed specific challenges in improving RTW of workers without an employment contract, sick-listed due to a CMD. One important challenge may be doubts about the sick-listed worker’s readiness to return to work. Our evaluation of the program’s execution in practice revealed not only that the participating professionals questioned the sick-listed workers’ RTW readiness but also the sick-listed workers themselves were sometimes insecure about their capabilities (36). This feeling of insecurity may reflect an anticipated stigma or fear-avoidance beliefs, both of which have been considered important risk factors for not returning to work (45, 46). Another challenge was the absence of a workplace to return to. The lack of a clear RTW perspective complicated translating experienced mental health problems into concrete obstacles for RTW and finding practical solutions to overcome these obstacles (36). Furthermore, many of the participants in our study were already unemployed before reporting sick, which may have increased their distance from the labor market.
The presence of an adverse intervention effect on the sickness benefit duration, found in the per-protocol group of our present study, was also visible in Vermeulen et al’s study (24), albeit not significant. In two ways, this finding can be related to SSA termination of OHC, once the sickness benefit ends. Firstly, intervention group participants, whose sickness benefit was likely to end soon after randomization according to the insurance physician, were excluded from participation in the new program as they were soon no longer entitled to OHC. As a consequence, the per-protocol group mainly consisted of participants whose sickness benefit was unlikely to end soon. Secondly, once participation in the program had started, the insurance physicians possibly first wanted to await the effectiveness of the new program before they terminated the sickness benefit.
Strengths and limitations of this study
A strength of this study is the assessment of both first sustainable RTW in paid employment and first RTW in any type of employment, which makes it possible to compare our results with results of multiple studies on RTW interventions. Moreover, our primary outcome may be considered robust because it only includes sustainable RTW (12, 24). Finally, the assessment of these outcomes with the use of both registered SSA and self-reported data, minimizes possible bias caused by self-report. A first limitation of this study is that, because of its pragmatic design, generalizing our results to other settings could be difficult. A second limitation is that we may have insufficiently addressed barriers for a successful execution of the participatory, supportive RTW program before the trial began. More comprehensive intervention mapping or a pilot study prior to the trial could possibly have helped to overcome some of these barriers. A third limitation of this study is the absence of blinding of both participants and professionals for the randomization result. A last limitation is that invitations for participation in the study were sent to a very large number of sick-listed workers (N=9822) to be able to include the necessary number of participants in this study as it was not possible to recruit participants solely based on a registered mental health problem (27).
Implications for practice and research
Based on the results of this study, we cannot recommend to implement the RTW program in the Dutch social security sector in its current form. Firstly, it will be necessary to overcome several barriers for a successful implementation. Secondly, it may be necessary to tailor the program to the specific needs and context of workers without an employment contract and sick-listed due to CMD. Lessons may be learned from successful RTW interventions aimed at people with more severe mental illness, such as supported employment. Part of this approach are regular meetings between all stakeholders, including employment specialists and healthcare providers (1). This approach is a good example of how to apply an integrated care approach so that treatment and vocational needs can be addressed simultaneously. Another characteristic of supported employment is ongoing support for both the worker and his/her employer during placement in work (1). Similar support may also stimulate early and sustainable RTW of sick-listed workers with a CMD and may be an incentive for employers to hire these workers. This may help to overcome barriers resulting from a limited availability of suitable jobs. Placement in a suitable job could further be stimulated by offering subsidized workplaces, as Vermeulen et al suggested earlier (24). Future research is needed to carefully consider these suggestions for developing a more suitable RTW intervention.
Concluding remarks
Compared to usual OHC, a participatory, supportive RTW program did not result in a significant shorter duration until sustainable RTW of workers without an employment contract and sick-listed due to a CMD. Nevertheless, due to implementation failure, it remains unclear what the results would have been if the program had been executed according to protocol. For future evaluation of a RTW program for this type of worker, it will be important to identify and overcome barriers for a successful implementation in an early phase. Further research may also be needed to consider how the vocational needs of these vulnerable workers could be better addressed.