In Japan, long working hours is an issue that needs to be addressed promptly for the sake of workers’ health. Karoshi (sudden death caused by cardiovascular or cerebrovascular disease due to overwork) and karojisatsu (suicide due to overwork) may also be related to working long hours. According to data from the Japanese Ministry of Health, Labor, and Welfare, the number of workers suffering from cardiovascular disease, cerebrovascular disease, and mental disorders due to work has increased by about threefold in the last decade (1, 2). Long working hours are common in many countries. According to statistics from the Organisation for Economic Cooperation and Development (OECD) on annual average working hours (3), Korea had the longest working hours between 1980–2007. However, in 2008, Korea dropped to second place behind Mexico. Similar to Japan, karoshi became recognized as a problem in Korea from the early 1990s (4) and consequently the number of working hours may deliberately have been reduced. An International Labor Organization (ILO) report (5) found that the proportion of workers working ≥49 or 50 hours/week in 2004–2005 was 49.5% in Korea, 23.6% in New Zealand, 20.4% in Australia, 18.1% in the US, and 14.7% in France. It also estimated that 22.0% of workers globally were working >48 hours/week.
Based on such data, many studies have examined the association between long working hours and health. Various outcomes such as all-cause mortality (6), disease (especially cardiovascular disease) (6, 7), biological indices [heart rate variability, blood pressure (BP), respiratory sinus arrhythmia, etc] (8–10), sleep (8, 9), depressive state (11), alcohol use (12), body mass index (8–10), fatigue (8–10), and general health status (13)have been investigated and positive, negative, or no association reported. The influence of long working hours on human health remains controversial, and we suggest that inconsistencies in the results are attributable to several factors such as the definition of long working hours, characteristics of participants, inclusion of shift work, measurement of outcomes, and potential covariates. In this systematic review, we mainly focused on excluding differences in the definition of long working hours and the influence of shift work.
Long working hours is recognized as working for a length of time which exceeds standard working hours. However, the definition of standard working hours may differ from country to country. For example, standard working hours are 35, 37, and 40 hours/week in France (14), Denmark (15) and the US (14), respectively. In Japan, the Labor Standards Law defines the maximum working time as 40 hours/week. The ILO Convention “Hours of Work to 40 a Week (C047)” was adopted in 1935 (16), but most countries, including Japan, have not ratified it. Under the European Union’s Working Time Directive (2003/88/EC), worktime, including overtime, was limited to 48 hours/week. The difference in standard working hours might affect the definition of long working hours in studies examining the association between long working hours and health. Consequently, this might influence the results of some studies. Therefore, we recognize that standard working hours are around 40 hours/week or 8 hours/day, and long working hours are defined as working longer than this. Moreover, in a study which investigates the association between long working hours and health, we believe that the results would be clearer and easier to understand when standard working time is used as the reference category in the analysis.
There are many types of shift work schedules, for example, night, irregular, and rotating shifts. Many studies have elucidated the association between shift work and health (17–22), and shift work is considered detrimental to health. Shift work has been associated with increased risk for myocardial infarction, coronary events, ischemic stroke (17), gastrointestinal symptoms, gastric ulcers (18), and metabolic syndrome (19). Female night-shift workers have also been reported to be at increased risk of breast cancer (20). Therefore, we must be careful when interpreting the results of studies with shift workers that investigate the association between working long hours and health. We believe that the statistical analyses in studies with shift workers need to be adjusted, by either excluding the shift workers from the analysis, stratifying the data according to work schedules, or adjusting for work schedules as covariates.
The purpose of this paper was to clarify the epidemiological evidence regarding the association between long working hours and health from previous studies by excluding differences in the definition of long working hours and the detrimental effect of shift work. Accordingly, we set our inclusion criteria and reviewed previous studies.
Methods
Search procedure
We conducted a systematic search of articles published in Medline and PsycINFO between 1995–2012 using the search terms: “work hours”, “workhours” “working hours”, “long hours,” “extended hours”, “overtime”, “overwork”, and “extended work”. Articles had to be published in English and peer-reviewed, with an abstract available. In the initial search, abstracts were checked for the inclusion criteria (see below). Next, fulltexts of the included articles were obtained and a detailed evaluation performed. The principal author conducted both the initial search and a detailed evaluation of the fulltext twice with an interval in between evaluations. Both authors analyzed those articles that finally remained.
Inclusion criteria
Study type
We included observational studies, such as prospective cohort, case–control, and cross-sectional studies. We excluded experimental and case studies, systematic reviews, meta-analyses, letters, and comments.
Participants
We included articles that did not incorporate shift workers, unless the statistical analysis was performed either by excluding shift workers, stratifying according to work schedules, or adjusting for work schedules as covariates. As described previously, we required a reference group that included participants working around 40 hours/week (8 hours/day) (ie, standard working time).
Working hours
The definition of working hours was time spent on work. Thus, we included hours of work brought home into the total working hours. The reason for this is that participants who worked outside the home but engaged in housework might go home with their work at a regular time (eg, 17:00 hours) but continue working at home. Working hours had to be described as working hours per day, week, or month. Otherwise, articles needed to indicate normal working hours (eg, working hours of contract) and the number of hours overtime. Similar to a previous review (23), we selected articles if the average working hours of participants exceeded 40 hours/week (8 hours/day), or average working hours plus one standard deviation (SD) were ≥40 hours/week (8 hours/day). This was because if the reference group included many participants with extremely short working hours, the effect of long working hours on health might be overestimated. Articles that covered compressed work weeks and temporarily busy periods were excluded.
Outcomes
The World Health Organization’s (WHO’s) definition of “health” is broad. In this review, we focused on outcomes that directly cause death or disease (eg, diagnosed diseases, sleep problems, depressive state or other psychologically disorders, and health-damaging behavior such as smoking). We excluded job satisfaction, job involvement, work–family conflict, well-being, quality of life, and work performance. We did not cover outcomes related to stress, such as the effort–reward imbalance or demand–control models and burnout. Accidents, injuries, and specific symptoms or illnesses related to work procedures were also excluded, because such outcomes might be specific to the job (eg, shoulder stiffness as a result of using visual display terminals).
Results
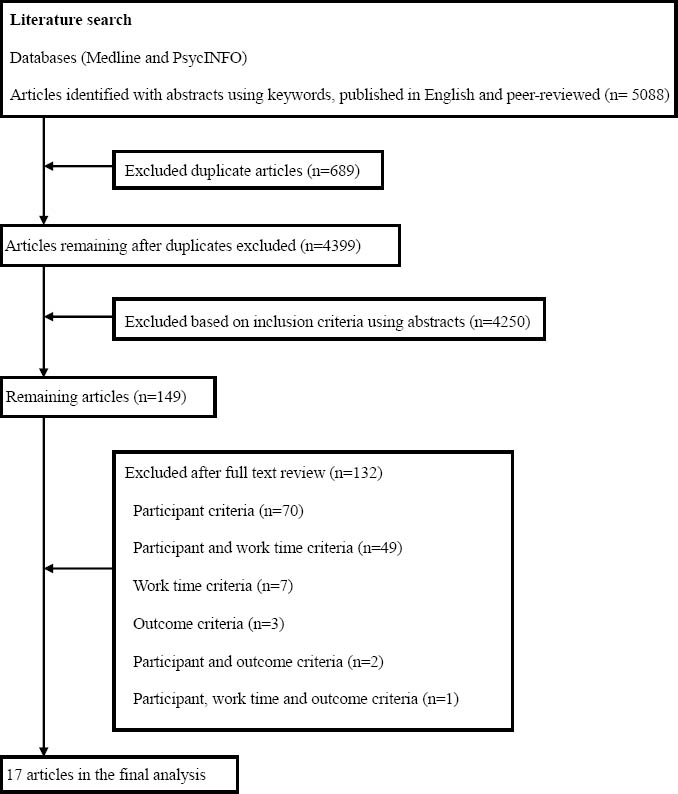
We identified a total of 5088 articles published in English and peer-reviewed with abstracts (figure 1). After excluding duplicates and reviewing abstracts, a detailed evaluation of the fulltext of 149 articles was performed. Finally, after taking inclusion criteria into consideration, 17 articles remained. Both authors examined these articles for details such as study design, characteristics of participants, working hours, definition and measurement of outcomes, statistical analysis, covariates, and results. Any disagreements were solved through discussion. When necessary, the authors of the articles were contacted.
In total, 19 studies (12 prospective cohort and 7 cross-sectional studies) were identified from the 17 articles, and a total of 32 outcomes are presented in table 1. The 19 studies are summarized briefly in tables 2 and 3. They are described in more detail in online Appendices A and B (http://www.sjweh.fi/data_repository.php).
Table 1
Category and number of outcomes from the final 17 remaining articles based on inclusion criteria. [BP=blood pressure; IFG=impaired fasting glucose]
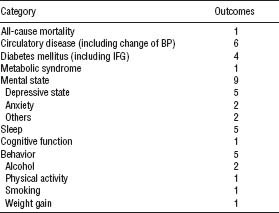
Table 2
Characteristics of 12 prospective cohort studies. [ADA=American Diabetes Association; ANCOVA=analysis of covariance; ANOVA=analysis of variance; CHD=coronary heart disease; CIDI=Composite International Diagnostic Interview; CoxPH=Cox proportional hazard analysis; dBP=diastolic blood pressure; DM=diabetes mellitus; GHQ=General Health Questionnaire; h/d=hours per day; h/m=hoursper month; h/w=hours per week; ICD-10=International Statistical Classification of Diseases and Related Health Behavior, tenth revision; IFG=impaired fasting glucose; LogRA=logistic regression analysis; MANCOVA=multiple analysis of covariance; MDE=major depressive episode; MI=myocardial infarction; ns=no association; sBP=systolic blood pressure; SD=standard deviation; Sig=significant; UMCIDI= University of Michigan’s version of the Composite International Diagnostic Interview; WHO=World Health Organization; (+)=positive association; (-)=negative association]
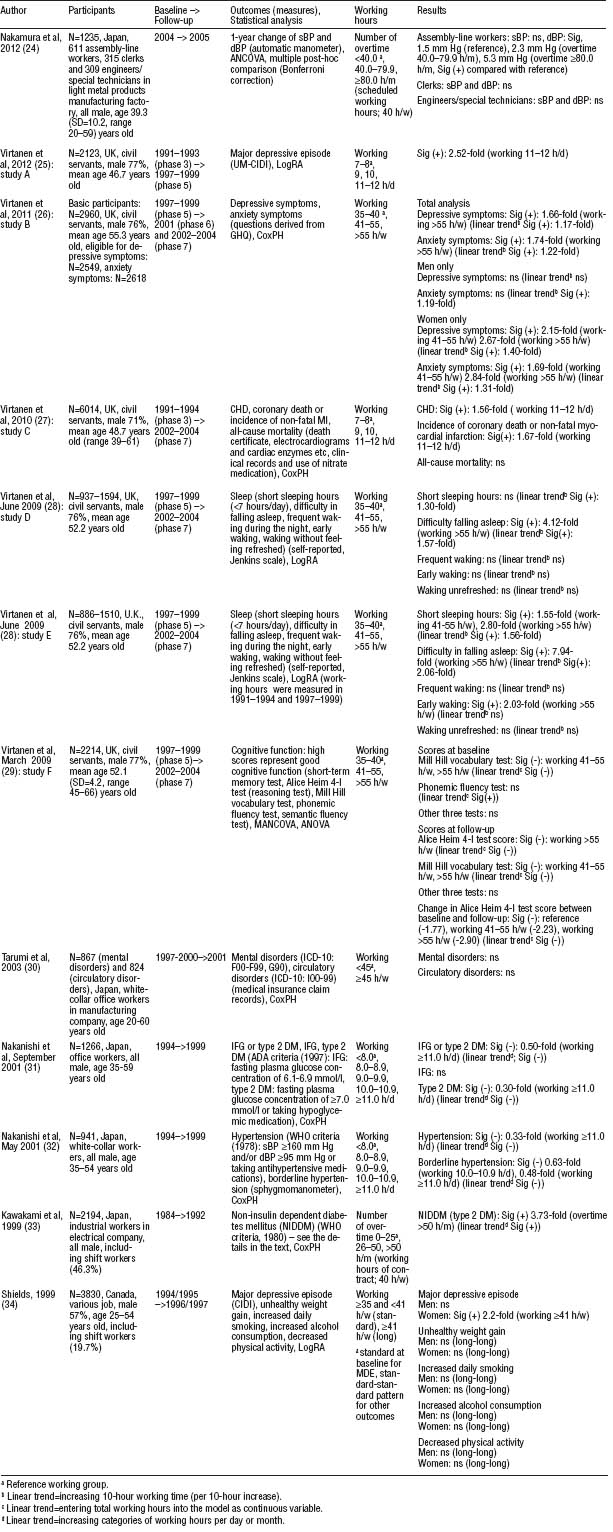
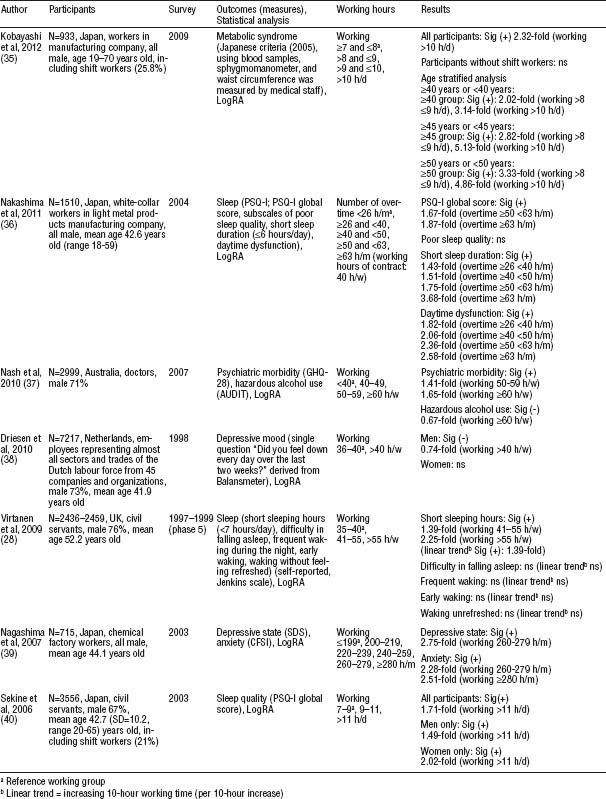
Table 3
Characteristics of seven cross-sectional studies. [AUDIT=Alcohol Use Disorders Identification Test; CFSI=Cumulative Fatigue Symptom Index; GHQ=General Health Questionnaire; h/d=hours per day; h/m=hours per month; h/w=hours per week; LogRA=logistic regression analysis; ns=no association; PSQ-I=Pittsburgh Sleep Quality Index; SDS=Self-Rating Depression Scale; Sig=significant; (+)=positive association; (-)=negative association]
Prospective cohort design
Nakamura et al (24) investigated the association between long working hours and one-year change in systolic and diastolic blood pressure (BP) among workers from the manufacturing industry. The average monthly hours of overtime were calculated from recorded timecards. Significant results were observed only among assembly-line workers. The one-year change in diastolic BP in the group working ≥80.0 hours/month of overtime was 5.3 mm Hg [95% confidence interval (95% CI) 2.7–7.9], which was significantly increased compared to that of the reference group [1.5 mm Hg (95% CI 0.8–2.2)].
Virtanen et al reported five articles (and six studies) (25–29) based on data from the Whitehall II study in the UK, which was established in 1985 with participants recruited from 20 London-based Civil Service departments. For convenience, we labeled the articles: Study A, 2012 (25), Study B, 2011 (26), Study C, 2010 (27), Studies D and E, June 2009 (28), and Study F, March 2009 (29). Since the article published in June 2009 (28) reported one cohort study with two different measurements for working hours, we treated this as two different studies (studies D and E). The measurement point of working hours was only at baseline in study D but twice in study E.
Study A (25) investigated the association between long working hours and the onset of major depressive episode (MDE) in the preceding 12-month period. Participants were followed for an average of 5.8 [standard deviation (SD) 0.4] years. MDE was evaluated using the University of Michigan’s version of the Composite International Diagnostic Interview (UM-CIDI), and the incidence was 3.1%. Participants in the group working 11–12 hours/day had a significantly increased risk of MDE [adjusted odds ratio (ORadj) 2.52 (95% CI 1.12–5.65)] compared to the group working 7–8 hours/day.
Study B (26) evaluated the effect of long working hours on mental health (depressive and anxiety symptoms). The mean follow-up period was 5.3 (SD 0.9) years for depressive symptoms and 5.2 (SD 0.9) years for anxiety symptoms. Outcomes were evaluated by subscales of the General Health Questionnaire (GHQ). The incidence was 2.0/100 person-years for depressive symptoms and 2.3/100 person-years for anxiety symptoms. The adjusted hazard ratio (HRadj) of participants in the group working >55 hours/week was significantly increased at 1.66 (95% CI 1.06–2.61) for depressive symptoms and 1.74 (95% CI 1.15–2.61) for anxiety symptoms compared to the group working 35–40 hours/week. Stratified analysis by gender was also conducted because of a significant interaction between working hours and gender. The significant results were one-sided for women.
Study C (27) was performed to investigate the association between long working hours and incidence of coronary heart disease (CHD) and all-cause mortality. The incidence of CHD included coronary death, incidence of non-fatal myocardial infarction, or incidence of definite angina pectoris. Participants were followed for an average of 11.2 (SD 2.7) years. The incidence of CHD was 5.46/1000 person-years. Participants in the group working 11–12 hours/day had a significantly increased risk [HRadj 1.56 (95% CI 1.11–2.19)] of developing CHD compared to the reference group. A similar increased risk was found for the outcome limited to coronary death or incidence of non-fatal myocardial infarction in the same group [HRadj 1.67 (95% CI 1.02–2.76)]. Long working hours were not significantly associated with all-cause mortality.
Studies D (28) and E (28) evaluated the association between long working hours and sleep condition. In study E, working hours were measured twice in 1991–1994 (before baseline) and 1997–1999 (baseline), and mean working hours were used in the statistical analysis. Outcomes were short sleeping hours, difficulty in falling asleep, frequent waking during the night, early waking, and waking without feeling refreshed. Participants in the group working >55 hours/week were at significantly increased risk for having difficulty in falling asleep: ORadj 4.12 (95% CI 1.71–9.94) and ORadj 7.94 (95% CI 2.97–21.25) in studies D and E, respectively. There were more significant associations in study E compared to D.
Study F (29) evaluated the association between long working hours and cognitive function. The study design had characteristics of both a prospective cohort and cross-sectional study. Participants were followed for a mean period of 5.5 (range 3.9–7.1) years. Five cognitive tests were conducted and high scores represented good cognitive function. At baseline, only Mill Hill vocabulary test scores of participants in the groups working 41–55 hours/week and >55 hours/week were significantly lower than those of the reference group. On the other hand, phonemic fluency test scores showed a significantly positive linear trend with working hours. At follow-up, Alice Heim 4-I test (reasoning test) scores of participants in the group working >55 hours/week and vocabulary test scores of participants in the groups working 41–55 hours/week and >55 hours/week were significantly lower compared to the reference group. Changes in reasoning test scores between baseline and follow-up showed a significant decrease among participants in the groups working 41–55 hours/week and >55 hours/week compared to the reference group.
Tarumi et al (30) surveyed the association between long working hours and mental disorders [International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10): F00-99, G90] and circulatory disorders (ICD-10: I00-99). Information on working hours was collected every year for four years and averaged working hours were used in the analysis. Incidence was 6.6/10 000 and 15.7/10 000 person-months for mental and circulatory disorders, respectively. After adjusting for covariates, no statistical significance was found.
Nakanishi et al conducted a cohort study, and reported two separate outcomes in articles published in September (31) and May (32) 2001. In this review, for convenience, we treated these as two separate studies.
The September article (31) evaluated the association between long working hours and impaired fasting glucose (IFG), on the one hand, and type 2 diabetes mellitus (DM), on the other hand. IFG and type 2 DM were diagnosed according to the criteria of the American Diabetes Association (1997) using blood samples or self-reported hypoglycemic medication use. Incidence was 24.1/1000 person-years for IFG or type 2 DM (15.0/1000 person-years for IFG, 9.1/1000 person-years for type 2 DM). The results showed a significantly decreased risk of IFG or type 2 DM for participants in the group working ≥11.0 hours/day [adjusted relative risk (RRadj) 0.50 (95% CI 0.25–0.98)]. No statistical significance was found for IFG, but a significantly lower risk was found for type 2 DM among participants working ≥11.0 hours/day [RRadj 0.30 (95% CI 0.09–0.94)].
Nakanishi et al’s other article (32) investigated the association between long working hours, hypertension (HT), and borderline HT. HT was defined according to the WHO criteria (1978) as: systolic BP ≥160 mm Hg and/or diastolic BP ≥95 mm Hg or taking antihypertensive medication. Borderline HT was defined as a BP between HT and normotension (systolic BP <140 mm Hg and diastolic BP <90 mm Hg). The incidence of HT and borderline HT was 19.4/1000 and 85.3/1000 person-years, respectively. The results indicated a significantly decreased risk among participants working long hours. For HT, participants in the group working ≥11.0 hours/day had a significantly decreased risk [RRadj 0.33 (95% CI 0.11–0.95)]. For borderline HT, participants in the groups working 10.0–10.9 hours/day and ≥11.0 hours/day had a significantly decreased risk [RRadj 0.63 (95% CI 0.43–0.91) and RRadj 0.48 (95% CI 0.31–0.74), respectively].
Kawakami et al (33) investigated the association between long working hours and non-insulin dependent DM (NIDDM, type 2 DM). NIDDM was diagnosed according to the WHO criteria (1980). An annual screening test using a urine sample was conducted for all participants. If glucosuria was found, fasting plasma glucose (FPG) was measured. Participants with high FPG (≥110 mg/dl) underwent a 75 g oral glucose tolerance test. The incidence for NIDDM was 1.95 /1000 person-years. The results indicated a significantly increased risk among participants working >50 hours/month of overtime [HRadj 3.73 (95% CI 1.41–9.90)].
Shields (34) conducted a survey to investigate the association between long working hours and MDE, weight gain, smoking, alcohol consumption, and physical activity. The incidence of MDE was 3% and 5% for men and women, respectively. The Shields’ study defined standard working hours as working ≥35–<41 hours/week, and long working hours as ≥41 hours/week. Results of MDE showed that only women working long hours had a significantly increased risk [ORadj 2.2 (95% CI 1.1–4.4)]. For the other four outcomes, this study took changes in working hours both at baseline and follow-up into consideration. In the statistical analysis, the reference group was defined as those working standard hours both at baseline and follow-up. The incidence for unhealthy weight gain, increased daily smoking, increased alcohol consumption, and decreased physical activity was 10% for both men and women, 9% for men and 7% for women, 34% for men and 25% for women, and 43% for men and 41% for women, respectively. This study showed the results of several working patterns, however, in this review, we dealt with those results with a “long-long” working pattern (working long hours both at baseline and follow-up) similar to other cohort studies. A “long-long” working pattern was not significantly associated with these four outcomes compared to the reference group.
Cross-sectional design
Kobayashi et al (35) investigated the association between long working hours and metabolic syndrome using Japanese criteria. Overall, prevalence was 11.8% among participants. This study conducted statistical analyses with or without shift workers (25.8%). The model without shift workers indicated no significant association with long working hours. On the other hand, the adjusted model with a shift work schedule showed a significantly increased risk among participants working >10 hours/day [ORadj 2.32 (95% CI 1.04–5.16)]. Several age-stratified analyses were conducted and indicated that those in the older age group with long worktime were at increased risk for metabolic syndrome compared to those of the same age in the reference group.
Nakashima et al (36) investigated the association between long working hours and sleep condition using the Pittsburgh Sleep Quality Index (PSQ-I). Working hours were recorded by timecards, and mean overtime of hours/month was calculated from data six months previously. A total of 35.8% of workers were above the PSQ-I cut-off point (poor sleepers). Poor sleepers and subscales of PSQ-I (poor sleep quality, short sleep duration, and daytime dysfunction) were analyzed. For poor sleepers, participants who worked ≥50 hours/month overtime had a significantly increased risk. The ORadj were 1.67 (95% CI 1.17–2.38) for ≥50 and <63 hours/month overtime and 1.87 (95% CI 1.30–2.68) for working ≥63 hours/month overtime. Short sleep duration and daytime dysfunction were significantly associated with long working hours. The more overtime participants worked, the greater the ORadj. Poor sleep quality was not significantly associated with the number of overtime hours worked.
Nash et al (37) surveyed the relationship between long working hours and psychiatric morbidity and hazardous alcohol use. Outcomes were measured by GHQ-28 and the Alcohol Use Disorders Identification Test (AUDIT). The prevalence of psychiatric morbidity was 28% and that of hazardous alcohol use was 15%. Participants working ≥50 hours/week were significantly more likely to suffer from psychiatric morbidity. The ORadj were 1.41 (95% CI 1.05–1.89) for working 50–59 hours/week and 1.65 (95% CI 1.20–2.26) for working ≥60 hours/week. For hazardous alcohol use, only the group working ≥60 hours/week had a significantly decreased risk [ORadj 0.67 (95% CI 0.45–0.99)].
Driesen et al (38) reported a survey from the Maastricht Cohort Study in 1998. In this review, we describe the association between long working hours and depressive mood according to our inclusion criteria. Depressive mood was assessed by the question, “Did you feel down every day over the last 2 weeks?” This wording was derived from the Balansmeter screening questionnaire. The prevalence was 6.8% for participants working 36–40 hours/week and 5.6% for those working >40 hours/week. The results were analyzed separately by gender because of a significant interaction between working hours and gender. A significant association was only found among men working >40 hours/week [ORadj 0.74 (95% CI 0.56–0.99)].
Virtanen et al (28) investigated the association between long working hours and sleep condition. This study used baseline data from the cohort study described previously (studies D and E), and outcomes were the same. Only short sleeping hours were significantly associated with long working hours. The ORadj were 1.39 (95% CI 1.16–1.68) for working 41–55 hours/week and 2.25 (95% CI 1.62–3.12) for working >55 hours/week.
Nagashima et al (39) reported a survey conducted on workers in 2003. In this review, we describe the association between long working hours, depressive state, and anxiety according to our inclusion criteria. Depressive state was measured by the Self-Rating Depression Scale (SDS) and anxiety was measured by the Cumulative Fatigue Symptom Index (CFSI). For depressive state, only participants in the group working 260–279 hours/month had a significantly increased risk [ORadj 2.75 (95% CI 1.39–5.46)]. For anxiety, participants working ≥260 hours/month had a significantly increased risk, ORadj 2.28 (95% CI 1.20–4.35) for working 260–279 hours/month and 2.51 (95% CI 1.29–4.90) for working ≥280 hours/month.
Sekine et al (40) reported the association between long working hours and sleep condition using PSQ-I. The prevalence of poor sleepers was 21.2% among men and 31.4% among women. All participants working >11 hours/day had a significantly increased risk [ORadj 1.71 (95% CI 1.28–2.29)]. Gender stratified analyses showed a significant risk among both genders: men working >11 hours/day [ORadj 1.49 (95% CI 1.03–2.15)] and women working >11 hours/day [ORadj 2.02 (95% CI 1.24–3.31)].
Discussion
In this review, we explored articles eligible for inclusion published between 1995–2012. We found a total of 17 articles and 19 studies and described the association between long working hours and health. We identified all types of associations (positive, negative, or none).
Outcomes
The articles included in our review dealt with various outcomes, thus, the relationship of each with long working hours was investigated.
All-cause mortality
Only one prospective cohort study (27) dealt with all-cause mortality. The results showed no significant association with long working hours. We could not reach any conclusion about this outcome due to the limited data available.
Circulatory disease
Four prospective cohort studies (24, 27, 30, 32) had six outcomes related to circulatory diseases. However, the results were inconsistent. Tarumi et al (30) indicated circulatory disorders including HT (ICD-10: I00-99) had no significant association with long working hours. We suspect that this result was affected by the small number of covariates (Appendix A: http://www.sjweh.fi/data_repository.php). Nakanishi et al (32) revealed that participants working long hours had a significantly decreased risk of HT and borderline HT. They described two reasons for these results: (i) whether the participants perceived overwork as stressful or not, and (ii) significantly higher 24-hour energy expenditure in the group working long hours. On the other hand, Nakamura et al (24) showed significantly increased diastolic BP in the group working ≥80.0 hours/month of overtime. We could not reach any conclusion regarding long working hours and BP.
The number of results related to CHD in our review were few and inconsistent (27, 30). However, in one meta-analysis about long working hours and CHD (41), these two articles (27, 30) were the basis for a subgroup analysis focusing on daytime workers. The results indicated an increased RR of 1.51 (95% CI 1.12–2.03) compared to those without long-term work. Thus, with the result of this meta-analysis, we concluded that working long hours is associated with CHD.
Diabetes mellitus
We found two studies (31, 33) that presented opposing results. Nakanishi et al (31) showed a significantly decreased risk associated with long working hours and the development of type 2 DM. However, Kawakami et al (33) indicated a significantly increased risk. Nakanishi et al (31) discussed the reasons for the discrepancy in great detail. They considered that it was caused by the difference in work environment and characteristics of participants, including the proportion of shift workers [0% (31) versus 46.3% (33)], the method of diagnosing DM, and high energy expenditure observed among participants working long hours (31). We agree with these suggestions, especially concerning the method of diagnosing of DM. Nakanishi et al (31) used blood samples and self-reported hypoglycemic medication use to diagnose DM, while Kawakami et al (33) used urine samples, blood samples, and 75 g OGTT. The latter would have been more accurate compared to the former. We also suspect that including shift workers among the participants made it more difficult to interpret the results. We found one meta-analysis which investigated long working hours and type 2 DM (42), but the results showed no association. Therefore, we could not reach any conclusion about the association between long working hours and DM.
Metabolic syndrome
We found one cross-sectional study (35) about metabolic syndrome. The results of the statistical analysis changed depending on whether shift workers were included or not. Only the results with shift workers showed a significantly increased risk. As mentioned in the introduction section, shift work is detrimental to health. We believe that further studies are needed with regards to this outcome.
Depressive state
We found five studies (25, 26, 34, 38, 39) about depressive state. One cross-sectional study (38) indicated that long working hours significantly decreased the risk of depressive mood. We believe that this finding resulted from the way in which the outcome was measured. In the study, depressive mood was evaluated by a simple question, similar to one of the criteria for MDE in the DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision) published by the American Psychiatric Association. However, it might be insufficient for measuring depressive mood. The reason is that patients themselves may not perceive they are experiencing a psychologically ill state, especially a depressive state. The other three prospective cohort studies (25, 26, 34) and one cross-sectional study (39) showed a significantly increased risk with long working hours. Consequently, we concluded that long working hours is associated with depressive state.
Anxiety
One prospective cohort study (26) and a cross-sectional study (39) investigated anxiety. Both results showed a significant increased risk for anxiety. We concluded that long working hours are indeed associated with anxiety. The results indicated that the risk rose among participants working >55 hours/week (26), 260–279 hours/month, or ≥280 hours/month (39). We suspect the existence of a threshold for developing anxiety.
Other mental states
We surveyed mental disorders (ICD-10: F00-99) in a prospective cohort study (30) and psychiatric morbidity in a cross-sectional study (37). We could not come to any conclusion about the association with long working hours due to the lack of data.
Sleep
We found five [two prospective cohort (28) and three cross-sectional (28, 36, 40)] studies that investigated sleep condition. A significant negative effect of long working hours on sleep condition was observed in all studies. We concluded that long working hours is associated with sleep condition.
In the two cohort studies (studies D and E) (28), study E identified more significant associations compared to study D. This might be attributable to the difference in measurement of working hours. Hence we consider that measuring working hours over a longer period is more effective to investigate the association between long working hours and health.
Two studies (36, 40) using PSQ-I to evaluate sleep condition presented similar results. This fact strongly supports the relationship between long working hours and sleep condition. All five studies had detailed subscales of sleep condition, and short sleeping hours or duration were highlighted regardless of the study design. Thus, among factors associated with sleep condition, short sleeping hours has been strongly associated with long working hours.
Cognitive function
We found one prospective cohort study (29) that evaluated cognitive function using five cognitive tests. However, one article was insufficient to enable us to reach any conclusion.
Behavior
We found one prospective cohort (34) and a cross-sectional (37) study examining behavior. Outcomes were alcohol use, physical activity, smoking, and weight gain. In the cohort study (34), no significant association was found between long working hours and the four outcomes. The cross-sectional study (37) showed a significantly decreased risk of hazardous drinking in the group working ≥60 hours/week. We inferred that the reason for this was the lack of personal time, which would in turn reduce the opportunity for drinking. From these results, we could not conclude any association between long working hours and health-related behavior.
However, one cohort study (34) revealed an important implication. In the results section, we only described the results of a long-long working pattern (working long hours both at baseline and follow-up) similar to other cohort studies. But participants with “standard-long” working patterns (working standard hours at baseline and long hours at follow-up) were at a significantly increased risk for alcohol consumption, smoking, and weight gain, compared to a “standard-standard” working pattern (working standard hours both at baseline and follow-up) (Appendix A, http://www.sjweh.fi/data_repository.php). Thus, a change in working hours from standard to long working hours could lead to an unhealthier lifestyle.
Summary and interpretation
We conclude that long working hours is associated with depressive state, anxiety, sleep condition, and CHD. Although compared to a previous review (23) we concluded that only a small number of health outcomes are associated with long working hours, we could clearly base our results on epidemiological evidence due to our strict inclusion criteria. To be more precise, due to our strict inclusion criteria, we were able to exclude differences in the definition of long working hours and the detrimental effect of shift work. By using the standard working group as the reference group, we believe we could find clearer evidence for the association between long working hours and health.
We aimed to exclude differences in the definition of long working hours and the influence of shift work for several reasons. Concerning the former, we found disparities in the definition of long working hours in previous studies and recognized this to be problematic because the results of each study were not easily comparable. Consequently, this could confuse the interpretation of the association between long working hours and health. By excluding differences in the definition of long working hours, it is easier to compare previous studies with each other. Furthermore, by comparing and unifying the results, we could reach a universal conclusion about these associations. With regards to the influence of shift work, we considered that this factor itself raised a health risk for workers (17–19). This has been implied by one meta-analysis (41) that investigated long working hours and CHD. The overall RR was 1.80 (95% CI 1.42–2.29) for long working hours. As described above, a subgroup analysis that was limited to daytime workers and did not include shift workers showed an RR of 1.51 (95% CI 1.12–2.03), lower than the overall RR. The exclusion of the influence of shift work seemed to decrease the health risk for long working hours and was, therefore, important in the studies about the association between long working hours and health.
We suspected that the health risk for long working hours in previous studies might confuse our interpretation unless appropriate consideration of the definition of long working hours and the influence of shift work was carried out. We strongly suggest future research that takes this into account when clarifying the association between long working hours and health.
Reasons behind the exclusion criteria
We identified 149 articles after our initial search. However, after a fulltext review, only 17 articles remained. The most common reason for exclusion was “participant criteria” (N=70), which concerned shift work and the reference group. Though we understand that each study has its own purpose and survey items differ according to the purpose, due to its detrimental effect on health, we believe that shift work has to be considered in the study design when evaluating the association between long working hours and health. From our search, only Kobayashi et al (35) presented results with and without shift workers. The significant negative impact on health observed among participants including shift workers disappeared in the results where shift workers were excluded. Even if statistical analyses are adjusted for work schedules, the influence of shift work may still partially remain.
Causal pathway
We have briefly inferred a causal pathway, which might explain why long working hours appear to increase the risk to health. Workers with long working hours need more time to recover from work (43). However, long working hours decrease the amount of private time available. Therefore, workers with long working hours do not have enough time to recover from exhaustion. The small amount of private time leads to an irregular lifestyle.
Such an irregular lifestyle may result in sleep problems and influence health-related behavior. If sleep problems, such as short sleeping hours and difficulty in falling asleep, continue for a given period, workers may develop lack of sleep, and insufficient sleep may lead to depression (44). Depression is a well-known risk factor for the development of CHD (45, 46). One meta-analysis (46) showed that subjects suffering from depression were at increased risk for developing CHD compared to non-depressed subjects. Short sleep time and frequent lack of sleep are also associated with an increased risk of acute myocardial infarction (7).
Irregular lifestyle caused by long working hours might also influence health-related behaviors such as alcohol consumption, smoking, and weight gain. From our search, we found that detrimental changes in health-related behaviors might occur when changes in working hours occur, such as changing from standard to long working hours (34). We suggest that these changes in health-related behaviors may cause a pre-morbid state, such as chronic liver or lung damage and the development of obesity, which in turn may lead to the development of diseases such as CHD and DM.
Limitations
The interpretation of our findings requires the consideration of several limitations. The first is selection bias. In our initial search, we used two databases with eight keywords. We selected peer-reviewed articles published in English with abstracts. Thus, articles that did not meet these requirements were not included in our review. The second limitation is publication bias. Although we examined many articles, there might be other studies that were not published because their results showed no significance. This might cause an overestimation about the relationship between long working hours and health. The third limitation is the measurement of working hours. Only two studies used timecards. We agree with the measurement of working hours using questionnaires or interviews because, in some cases (31, 32), participants who hold managerial positions may not record their working hours using a time clock. However, self-reported working hours may also be inaccurate.
Concluding remarks
Our systematic review concluded that long working hours is associated with depressive state, anxiety, sleep condition, and CHD. Though the number of health outcomes we ascertained was small due to our strict inclusion criteria, we were able to exclude differences in the definition of long working hours and the influence of shift work. Since both factors may influence the association between long working hours and health, further studies are necessary that deal with them appropriately.