Due to the ageing workforce and decreasing birth rates, it has become crucial to ensure older employees work productively and in good health for longer. Alongside ageing, health problems occur more often and in turn work ability can decrease (1). Poor health can lead to reduced productivity in terms of productivity loss at work, increased sickness absence, or exit from the workforce (2–4). The influence that poor health has on sickness absence differs for various types of health problems (3–5). Work-related factors, such as autonomy, social support, and work pressure also influence productivity loss at work and sickness absence (6–9). Past findings indicate that work-related factors, such as autonomy, job satisfaction, physical load, and social support, interact with health problems in their influence on productivity outcomes (10–14).
In accordance with past findings, we hypothesize that favorable factors at work such as high support, high autonomy, low job and emotional demands, and low physical load can help employees with health problems to remain productive at work and avoid or reduce sickness absence. Findings from past qualitative research (15, 16) support the idea that work-related factors modify the effect of health on sickness absence, but quantification of this occurrence is still lacking in the literature. Understanding the effect of work on the influence of poor health on sickness absence has important practical implications because health problems may not always be solved, but work-related factors are amendable.
Since past studies have shown that different health problems affect sickness absence to a different extent (3, 5), it is possible that effect modification of work-related factors also differs per health condition. We hypothesize that health problems will cause sickness absence if unfavorable work factors are present that trigger or aggravate the health problems or that interfere with functioning. For example, psychosocial work factors such as emotional demands and lack of support could especially modify the effects of psychological health problems on sickness absence, whereas workers with musculoskeletal disorders in physically demanding jobs may experience more limitations at work and, thus, are more likely to call in sick. Gaining such problem-specific insight is essential for the development of tailored interventions for sustainable employability, defined as maintaining a high work productivity in good health. The goals of this study were to (i) assess how health problems and work-related factors predict sickness absence and (ii) investigate whether and to what extent work-related factors modify the effects of common health problems on sickness absence.
Methods
Study design
A prospective study with a one-year follow-up was conducted within the longitudinal Study on Transition in Employment, Ability, and Motivation (STREAM) (17). In STREAM, a stratified sample of Dutch citizens aged 45–64 years complete annual online questionnaires on health, job and personal characteristics, work ability, productivity, and transitions in employment. The current study used STREAM data from 2010 (baseline) and 2011 (follow-up). In 2010, 15 118 individuals participated (response 71%), with comparable participation in the four age groups sampled: 45–49, 50–54, 55–59, and 60–64 years. In 2011, 12 430 individuals participated again in STREAM (82%). As our research questions pertained to work-related factors that are specific to workplace settings, we excluded participants if they underwent a transition in work status (employed, self-employed, not employed) between baseline and follow-up (N=1075), were self-employed both years (N=728), or not employed both years (N=1474). Of the remaining participants, 169 persons were excluded because of incomplete data, resulting in a total inclusion of 8984 participants in this study.
The Medical Ethical Committee of the Free University of Amsterdam Medical Center declared that the Medical Research Involving Human Subjects Act does not apply to the STREAM study. The Medical Ethical Committee had no objection to the execution of this research. In the information that accompanied the online questionnaire, it was emphasized that (i) the privacy of participants was guaranteed, (ii) all answers to the questions were anonymous and would be treated confidentially, and (iii) all data were stored in secured computer systems.
Sickness absence
Sickness absence was assessed at baseline and at follow-up with the open question: “How many work days have you, during the past twelve months, been absent due to sickness?” Three categories of cumulative sickness absence were made: none (0 days), low (1–9 days), and high (>9 days).
Health problems
The occurrence of various health problems at baseline was assessed with the question: “Do you [currently] have one or more of the following chronic diseases, disorders, or handicaps?” (18). Of the 13 answer options, the following 7 categories were made: musculoskeletal disorders (MSD), migraine or severe headaches, circulatory diseases, respiratory diseases, digestive problems, diabetes, and psychological complaints. These health categories were not mutually exclusive. Multimorbidity was defined as the presence of ≥2 health problems.
Work-related factors
Studied work-related factors included: autonomy, support, job demands, emotional demands at work, and physical workload. Autonomy was measured with five items derived from the Job Content Questionnaire (JCQ) about: making decisions, deciding the order of and speed of conducting tasks, having to find solutions, and being able to take time off (Cronbach’s alpha=0.78) (19). Job demands, measured with four JCQ items, consisted of how fast, much, hard, and hectic an individual’s work is (Cronbach’s alpha=0.87) (19). Support was measured with four items from the Copenhagen Psychosocial Questionnaire (COPSOQ) concerning whether colleagues and supervisors are willing to help and listen to work-related problems (Cronbach’s alpha=0.81) (20, 21). Emotional demands at work were also assessed with three items derived from the COPSOQ about emotionally difficult situations, emotional demands, and emotional involvement at work (Cronbach’s alpha=0.85) (20, 21). Physical workload was assessed with five items from the Dutch Musculoskeletal Questionnaire on force exertion, static load (standing, posture, kneeling), and vibration (using tools or machines that cause vibration) (Cronbach’s alpha=0.86) (22). All work-related factor items had 5-point answer scales ranging from 1=(almost) never to 5=always. These scales were dichotomized based on the sample distribution (median values). Categories suspected of having the lowest risk for sickness absence were used as reference categories (23).
Covariates
Age, gender, and educational level were incorporated in this study as covariates. The highest level of education attained was categorized into three groups: low (lower general secondary educational, preparatory secondary vocational education), medium (intermediate vocational training, higher general secondary education, pre-university education), and high (higher vocational education, university education).
Statistical analysis
Descriptive statistics were used to report on general characteristics of the study population. Multinomial logistic regression analyses were conducted to study associations between health problems and work-related factors as independent variables at baseline with the occurrence of cumulative sickness absence during 12-month follow-up, distinguishing none (0 days) (reference), low (1–9 days), and high (>9 days) cumulative sickness absence. Odds ratios (OR) and their corresponding 95% confidence intervals (95% CI) were calculated. First, in model 1, analyses were conducted for each independent variable separately, adjusting for age, gender, and education, since these individual characteristics were significantly related to sickness absence. Thereafter, a multivariate analysis (model 2) using an enter method was conducted, incorporating the work-related factors, health problems, and covariates that had a significant association with either low or high cumulative sickness absence in model 1. This procedure allows for a direct comparison between determinants of low and high sickness absence. Lastly, in model 3, baseline sickness absence was also added to the multivariate model, categorized the same way as follow-up sickness absence. This model focuses on incidence rather than occurrence of sickness absence as the dependent variable. As multimorbidity was defined on the basis of separate health problems, this variable was not included in either models 2 or 3 in order to avoid over adjustment.
To study whether and to what extent work-related factors modified the effect of health problems on sickness absence, interaction effects were analyzed by calculating relative excess risk due to interaction (RERI) terms and their 95% CI, using the delta method in Excel (Microsoft Corp, Redmond, WA, USA) (23–25). RERI are calculated with OR as estimates of relative risks (RR), RERI= OR(health problem + unfavorable work factor) – OR(health problem + favorable work factor) – OR(no health problem + unfavorable work factor) + 1 (23, 24). When RERI is not equal to zero, an additive interaction is present; RERI can range from negative infinity (negative interaction, less than additivity) to positive infinity (positive interaction, more than additivity) (23). Through this analysis the per cent increase in likelihood of sickness absence for persons with a health problem and unfavorable work-related factors as opposed to those with the health problem and favorable work-related factors was also calculated [((ORhealth problem + unfavorable work factor – ORhealth problem + favorable work factor)/ORhealth problem + favorable work factor) × 100]. Variables that were significantly related (P<0.05) to sickness absence in the multivariate analysis (model 2) were incorporated in the effect modification analyses. Analyses were done using SPSS, version 20, (SPSS Institute, Chicago, IL, USA) and Excel.
Results
Descriptive information
The study population characteristics can be found in table 1. Loss-to-follow-up was 18% for both men and women, 20% and 17% for the youngest and the oldest age groups, respectively, and 18% and 16% for low and high educated persons, respectively. Persons with high baseline cumulative sickness absence had a loss-to-follow-up of 18%, this was 17% for those with a low sickness absence.
Table 1
Demographic, health, work, and sickness absence descriptive information among N=8984 employed older (aged 45–64) individuals.
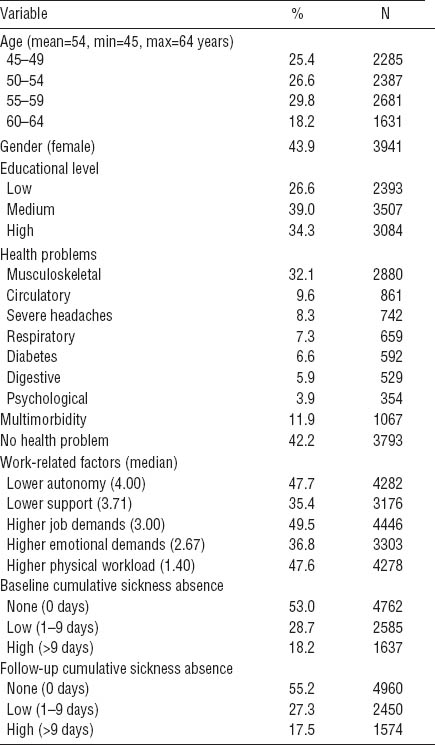
Additional analyses showed that, at baseline, men were less likely than women to have cumulative sickness absence of 1–9 days [OR 0.87 (95% CI 0.79–0.96) and of >9 days [OR 0.90 (95%CI 0.80–1.01)]. The oldest age group had less sickness absence of 1–9 days [OR 0.58 (95% CI 0.50–0.67)] but similar sickness absence of >9 days [OR 0.94 (95% CI 0.79–1.13)] when compared to the youngest age group. Lower educated persons were more likely to have high [OR 1.43 (95% CI 1.24–1.65)] and less likely to have low [OR 0.76 (95% CI 0.67–0.86)] cumulative sickness absence. All covariates were included in the remaining analyses.
More than fifty per cent of the participants were not absent during the one-year follow-up, about 27% had a short cumulative sickness absence (1–9 days) and about 17% had high cumulative sickness absence (>9 days) within the past year. The prevalence of sickness absence at baseline was 47% and 45% at follow-up. For both low and high sickness absence, the recurrence was approximately 46% and the incidence approximately 17%.
By far the most frequently present health problem at baseline was a MSD (32.1%), followed by circulatory diseases (9.6%), and severe headaches (8.3%). The same pattern was seen in the frequency of health problems at follow-up, the maximum change in prevalence between the two assessments was 0.8%. Multiple health problems were present in 11.9% of the study population at baseline, often combinations of MSD with:



