In today’s Western societies, only a quarter of the labor force works regular 9–5 office hours, while the remainder is engaged in shift work or has irregular work hours (1). More often than day workers, shift workers report mental health symptoms, such as fatigue, nervousness, anxiety, and depressed mood; they also use sleeping pills and tranquillizers more often (2, 3). Shift workers may experience sleep problems when the circadian rhythm promotes alertness. Short or poor sleep leads to insufficient recovery and stress (4, 5). However, disturbed sleep is not the only pathway between shift work and mental health. Some neuroendocrine mechanisms may contribute to depressed mood among shift workers. Shift work reduces glucocorticoid sensitivity of the peripheral tissues, resulting in functional hypercortisolism (6). Glucocorticoid resistance and hyperactivity of the hypothalamic-pituitary-adrenocortical axis play a role in the pathogenesis of depression and other psychiatric disorders (7). Shift work also disturbs nocturnal melatonin secretion, and reduced endogenous melatonin levels have been associated with the onset of depression and anxiety disorders (8).
Besides disturbed sleep and neuroendocrine mechanisms, psychosocial pathways could explain why shift workers experience more mental health symptoms than day workers (3, 9). Shift work interferes with participation in family life and alienates workers from their social environment by desynchronization from daily societal habits. Haines et al (10) estimated that 70% of the effect of shift work on depression is direct and 30% is mediated through work–family conflict and social desynchronization.
The fact that shift workers experience mental health problems more often than day workers does not necessarily imply they are off work due to mental disorders more frequently. Merkus et al (11) found inconclusive evidence for increased sickness absence (SA) levels among shift workers. A variety of health-related and decisional theories try to explain why workers report sick in a particular case. The threshold of taking sick leave may differ between shift and day workers. For example, shift workers may refrain from reporting sick when they think it will be difficult to find substitutes. We found no epidemiological studies that investigated SA due to mental disorders among shift workers. The objective of this observational study was to compare shift and day workers for risk of mental health SA, addressing the research questions: (i) Do shift workers have a higher risk of mental health SA than day workers? (ii) Do shift workers have a higher risk of recurrent mental health SA than day workers?
Methods
Study population
The study population consisted of 6678 male production workers employed at a steel mill. SA data were retrieved from an occupational health service (OHS) register and work schedules were obtained from the employer’s payroll. Baseline was set at 1 January 2002 and workers were followed until 31 December 2011. We excluded workers whose shift schedules were not available (N=527) or differed from a 5-shift schedule (N=107); 218 workers were excluded because they had had mental health SA in the two years prior to baseline. Consequently, the data of 5826 male production workers were analyzed: 4288 (74%) shift workers with a forward rotating 5-shift schedule MMEEXNNXXX (M=morning 06:00–14:00 hours, E=evening 14:00–22:00 hours, N=night 22:00–06:00 hours, and X=day off) and 1538 (26%) day workers (08:00–17:00 hours). During follow-up, 1484 (1084 shift and 400 day) workers left employment; the mean (standard deviation) follow-up period was 7.7 (3.0) years. The Medical Ethics Committee of the University Medical Center Groningen granted ethical clearance for this register-based study.
Mental health SA
SA was defined as a financially compensated temporary leave from work due to work-related and non-work-related injuries and illness. In the Netherlands, SA is employer-compensated when medically certified by an occupational physician (OP) within 42 days of reporting sick. SA certified within the International Classification of Diseases (ICD-10) categories of emotional disturbance (ICD-10 R45) or mental and behavioral disorder (ICD-10 F00–F99) was defined as mental health SA. Recurrent mental health SA was defined as any mental health SA episode occurring >28 days after recovery from the first mental health SA episode since January 2002.
Statistics
All analyses were performed with SPSS Statistics version 20 (IBM, Armonk, NY, USA). The risks of incident and first recurrence of mental health SA were analyzed with Cox regression including work schedule (shift versus daytime) as independent variable with age (continuous variable) and occupational grade (discrete variable, 1=unskilled, 2=semi-skilled, 3=skilled steel workers, 4=maintenance technicians, and 5=supervisors) as covariates.
During the study period, 386 workers changed their work schedule: 292 from shift to day work and 94 from day to shift work. Ten percent of the workers who changed their work schedule had mental health SA as compared with 8% of those who did not change their work schedule. Information on why workers changed their work schedule was not available. To exclude potential interactive effects between mental health SA and work schedule, we performed a sensitivity analysis including the 5440 (3996 shift and 1444 day) workers who did not change their work schedule during the study period.
Results
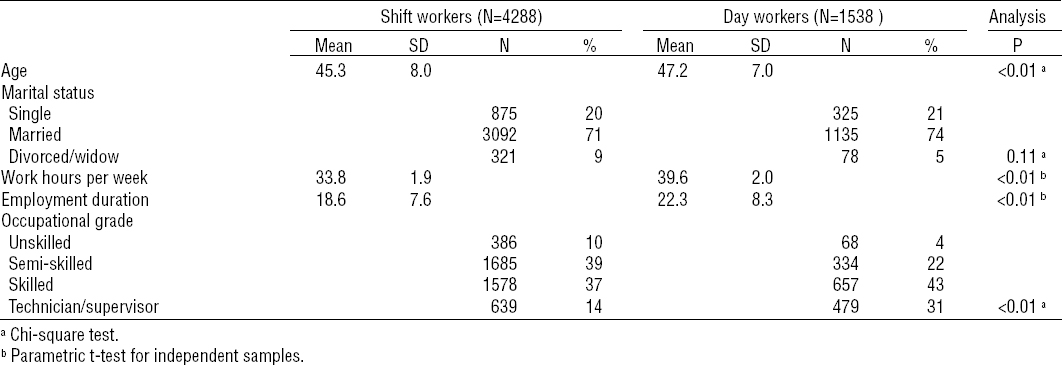
Day workers were older and worked more hours/week in higher grade jobs than shift workers (table 1).
Table 1
Baseline characteristics of the study population of male production workers (N=5826). [SD=standard deviation]
In total, 477 (351 shift and 126 day) workers had mental health SA. Shift workers had no increased risk of incident mental health SA [hazard ratio (HR) 1.03, 95% confidence interval (95% CI) 0.84–1.26] compared with day workers. Shift workers had higher risks of SA due to mood and neurotic disorders, although the difference between shift and day workers was not significant (table 2).
Table 2
Risk of mental health sickness absence (SA). The table shows mental SA stratified by ICD-10 diagnosis and hazard ratios (HR) with related 95% confidence intervals (95% CI) of Cox regression analysis, adjusted for age and occupational grade; HR>1 reflects higher and HR<1 lower risk of mental health SA among shift compared with day workers.
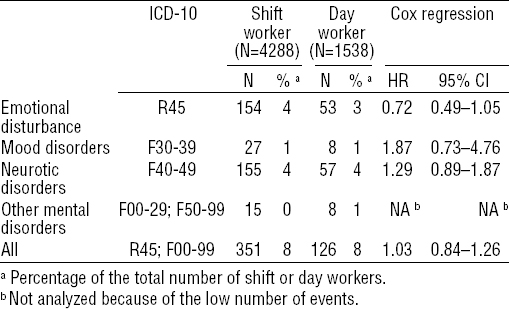
Of the 477 workers who had had mental health SA, 117 (96 shift and 21 day) workers had recurrent mental health SA. Shift workers had no increased risk of recurrent mental health SA (HR 1.04, 95% CI 0.62–1.74) compared with day workers.
Sensitivity analysis
Of the workers with no change in work schedule, 357 (251 shift and 106 day) workers had incident and 107 (86 shift and 21 day) workers had recurrent mental health SA. The risks of incident (HR 1.19, 95% CI 0.88–1.60) and recurrent (HR 0.83, 95% CI 0.48–1.43) mental health SA did not differ between shift and day workers.
Discussion
Our 10-year observational study showed that shift workers did not have a higher risk of incident and recurrent mental health SA than day workers. The risk of incident SA due to mood disorders was higher among shift than day workers but did not differ significantly. The statistical power of a Cox regression model including 3 independent variables and 27 events (ie, SA episodes due to mood disorders) is debatable, although Vittinghoff and McCulloch (12) showed that CI coverage, type I error, and relative bias with 5–9 events per variable were comparable to those with 10–16 events per variable. In a previous Dutch study, Driessen et al (13) found a higher risk of depressed mood among male and actual shift workers as compared with female and former shift workers, but the results were no longer significant when educational level and psychosocial work factors were controlled for.
Selection issues
Shift workers may represent a relatively healthy part of the working population. This healthy worker selection starts with the worker’s judgement of his ability to withstand shift work and may be reinforced by pre-placement medical assessments (14). Healthy worker selection then continues in terms of a survival effect in which less healthy shift workers are likely to transfer to daytime work or quit the job. We had no information about pre-employment selection mechanisms and could not identify which day workers were former shift workers because payroll data from before January 2000 were not available. The sensitivity analysis including only the workers with the same schedule throughout the 10-year study period confirmed the finding that the risk of mental health SA did not differ between shift and day workers.
Methodological considerations
Although the use of OP-recorded ICD-10 diagnoses restricted recall and social desirability bias, the reliability of OP-diagnoses is being debated. O’Niell et al (15) found no systematic difference between OP and psychiatrists in their diagnostic labelling of mental ill-health, although within-group reliabilities were low for some diagnoses, particularly ‘stress’. We limited potential diagnostic misclassification by using main ICD-10 (eg, ‘neurotic disorders’) instead of specific (eg, burnout, adjustment disorder, or anxiety disorder) diagnoses.
All workers were employed at the same company. Consequently, differences in mental health SA could not be attributed to organizational policies and practices. The study population is a convenience sample, which may not be representative of the general working population. Furthermore, only men working in a forward-rotating 5-shift schedule were included. The results might not generalize to female shift workers (eg, in healthcare) and workers engaged in other shift systems.
Concluding remarks
We conclude that the risk of incident and recurrent mental health SA did not differ between shift and day workers. Larger-scale studies are required to differentiate between the mental health effects of shift work and mental health SA diagnoses. Furthermore the relationship between shift work and SA due to mood disorders should be examined in more detail.



