Excessive time spent sitting has been linked to adverse health outcomes (1–4). High levels of sitting time are now common, particularly in desk-based workplaces, where occupational environmental, social and technological changes have facilitated or mandated this behavior (5, 6). To address this emergent work health and safety issue (7), the use of sit-stand workstations, combined with other workplace strategies, are increasingly being trialed, with findings showing that substantial short- and medium-term reductions in workplace sitting time can be achieved (8–11). There is also interest in potential benefits that may accrue to organizations, such as reduced absenteeism (12). The cost implications of sit-stand workstations have been identified as a potential barrier to widespread uptake (13, 14), however to date, there is no published evidence of the cost-effectiveness of such interventions. It is useful to determine whether up-front set-up costs, including acquisition and installation of sit-stand workstations, are balanced by health and workplace benefits as well as future healthcare savings that potentially result from the intervention.
The “Stand Up Victoria” study was a cluster-randomized controlled trial (RCT) that evaluated the effectiveness of a multi-component intervention involving environmental (including sit-stand workstations), organizational and individual-level approaches aimed at reducing workplace sitting time among desk-based workers (12). Compared to a usual practice control group, there were significant changes (all favoring the intervention) for both workplace and overall sitting and standing time at the 12-month follow-up.
This economic evaluation is reported as a distinct follow-up to the main findings given the following reasons: (i) the design of the economic evaluation (ie, designed a priori with its own hypotheses); (ii) the importance of findings to guide policy-making in the field of workplace occupational health & safety; and, (iii) the significant distinctions from previous workplace physical activity economic-evaluation studies in that it incorporates both within-trial economic analysis and modelling of the long-term health outcomes beyond the trial duration).
It is of broader public and occupational interest to assess the health economic credentials of this intervention to justify the resource allocation and inform decisions about scaling up for more widespread delivery. Using both within-trial economic analysis, as well as modelling the long-term health outcomes beyond the trial duration, we assessed whether the intervention used in Stand Up Victoria could be cost-effective in improving the long-term health of office workers.
Methods
Intervention
Stand Up Victoria was conducted in 14 worksites within the same organization between 2012–2014. Worksites were randomized to either: a 3-month active multi-component intervention followed by a 9-month passive follow-up period; or to a usual practice control condition. Trial design (12), worksite characteristics (15), activity outcomes (16), and cardio-metabolic outcomes (8, 17) have been published elsewhere.
Data collection
Assessments occurred at baseline, 3 months (immediately post-intervention) and 12 months post-baseline, and included activity monitoring (using the activPAL3™ activity monitor, PAL Technologies Limited, Glasgow, UK; minimum version 6.3.0), an onsite objective health assessment (including body composition measures), and a self-administered online questionnaire (16).
Economic evaluation
This economic evaluation entailed two steps. First, a within-trial analysis was conducted alongside the trial, to determine the intervention’s cost-efficacy in terms of reducing workplace sitting time. Second, a multi-state Markov model was used to evaluate the intervention’s cost-effectiveness if delivered to the eligible Australian population and the observed intervention effect was extrapolated over the cohort’s lifetime.
Both analyses adopted a societal perspective which took into account costs to government as a third-party provider of healthcare services in Australia and the costs to private organizations implementing the program within their workplaces. All costs were reported in 2014 Australian dollars (1 AU$ = 0.943 US$ June 2014) and analyses were performed on an intention-to-treat (ITT) basis.
Cost-efficacy analysis: within-trial economic evaluation
An incremental cost-efficacy analysis, undertaken according to a pre-specified economic protocol, measured the net costs and net efficacy of the intervention compared to usual practice.
Outcomes
The primary outcome was total workplace sitting time standardized to an 8-hour day. Secondary activity outcomes were prolonged sitting (sitting time accrued in bouts ≥30 minutes), standing, and stepping time at the workplace (per 8-hour workday), and overall time per 16-hour waking day spent sitting, standing and stepping (16). Other secondary outcomes considered for this analysis were body mass index (BMI), self-reported health-related quality of life (measured by Assessment of Quality of Life-8D; AQoL-8D) (18), and work days lost (absenteeism). The time horizon for the measurement of benefits was the 12-month intervention duration.
Absenteeism based on days of sick leave taken for periods one year prior to (period 1) and one year during the study (period 2) were extracted for each participant from the human resources database of the participating sites. Participants not employed by the organization during period 1 were excluded from this analysis (N=18). The absenteeism cost was estimated based on the change in unplanned absence days claimed between periods 1 and 2.
Data analysis
The between-group difference in changes of sick leave (expressed in days) was compared using linear regression given the near normal distribution of the raw data. For other efficacy outcomes, similar statistical methods were adopted to determine the intervention effects and changes within groups. Outcomes were log transformed as required to improve normality and/or reduce heteroscedasticity. Detailed methods are reported elsewhere (16). Missing data were dealt with via multiple imputation, assuming all missing-at-random (MAR). The imputation model (m=20 imputations) included all the variables used in the analysis for corresponding outcomes, a fixed effect for cluster (N=12), and any other variables that showed an association with the odds of the missing data at P<0.2 (16).
Analyses were performed in STATA version 14 (StataCorp LP, College Station, TX, USA) with statistical significance set at P<0.05, two-tailed. The differences between groups in terms of activity outcomes, BMI, AQoL-8D, and unplanned absence days were adjusted for potential confounders (age, gender) and baseline workplace sitting time.
Costs
Pathway analysis was used to identify the resource items associated with the intervention’s implementation (supplementary table S1, www.sjweh.fi/show_abstract.php?abstract_id=3740). The intervention was assumed to be running in steady state and operating at its full effectiveness potential; time spent on intervention design and planning was excluded. Resource use was recorded as part of the process evaluation. Costs of the sit-stand workstations were annuitized over five years. Official schedules of unit costs (such as Medicare Benefits Schedule fees, see supplementary table S1) were sourced where appropriate. In the intervention group, total cost comprised the cost of intervention delivery with or without the cost of adverse events attributable to the intervention (supplementary table S2, www.sjweh.fi/show_abstract.php?abstract_id=3740). No costs were assumed in the usual practice control group.
Cost-efficacy analysis
Incremental cost-efficacy ratios (ICER) were calculated as the difference in costs of the intervention and usual care divided by the difference in their effect, where the efficacy outcomes were considered to be significantly different between groups (P<0.05). The primary ICER was expressed as the cost per unit (minutes per 8-hour workday) reduction in workplace sitting time at 12 months. Secondary outcomes were cost per unit reduction/change at 12 months in: (i) overall sitting time (per 16-hour day); workplace standing time (per 8-hour workday); stepping time (physical activity) (per 8-hour workday and per 16-hour day); (ii) BMI; (iii) health-related quality of life measured by AQoL-8D (18); and, (iv) absenteeism.
Uncertainty and sensitivity analyses
Three separate sensitivity analyses were undertaken to quantify the uncertainty surrounding the ICER to check the robustness of the results and critical roles of different parameters when key variables or assumptions are varied: (i) the upper and lower limits of individual variables including the unit costs of facilitator and sit-stand workstation set up, were tested; (ii) the costs of the sit-stand workstations were not annuitized; and (iii) to complete the ITT results, cost-efficacy outcomes were analyzed using the study completers’ dataset.
Cost-effectiveness analysis (CEA): modelling of long-term health outcomes and costs
Outcomes and costs
The cost-effectiveness analysis (CEA) extended both the timeframe for measuring costs and benefits and the population receiving the intervention. While based on the intervention effect at 12 months, outcomes and costs were measured over the cohort’s lifetime from the 2014 reference year. In the absence of evidence, intervention effects were assumed to decay over the five-year period post intervention. The CEA was modelled for the trial population and also extrapolated up to the eligible national population.
For the national roll-out, it was conservatively assumed that one fifth of the 45% of Australians who work in a sedentary occupation would take up the intervention (19). This assumption was based on the premise that most of the associated costs would be borne by employers and that not all workplaces would be in a position to incur them. Some additional costs were factored in to facilitate national delivery of the intervention. It was hypothesized that each of the seven Australian states plus the Northern Territory would require one officer to coordinate the intervention’s implementation at the state level.
All future health outcomes and costs were discounted at 3% per annum (20). An existing multi-state life table Markov model was used to estimate the effect of changes in BMI or physical activity independent of BMI on health outcomes and healthcare costs of nine diseases causally related to obesity. It simulates and compares a reference population [with the BMI distribution (21) and disease pattern of the Australian population in the year 2010 (22, 23)] to an intervention population (which is identical except that it receives the intervention). Where there was a significant difference between groups for activity outcomes (ie, additional standing or stepping time replacing sitting time), the difference in time (expressed in minutes) was multiplied by the difference in metabolic equivalent units (MET) of the particular activity compared to sitting. The consequences of a change in BMI and/or physical activity across age-sex groups were estimated by applying potential impact fraction calculations with continuous exposure and risk functions to disease incidence. Changes in incidence resulted in changes in future prevalence and disease-specific mortality for the cohort. The health benefits of the intervention are modelled as a reduction in incidence of each obesity-related disease. Each disease is modelled with four health states (healthy, diseased, dead from the disease, and dead from all other causes). This model has been used in a number of published economic evaluation (24–26). Further details of the Markov model can be found elsewhere (24–26). Disease treatment costs were drawn from the Australian Institute of Health and Welfare/ The model was built in Excel (Microsoft Office 2003) and uses the add-in tool Ersatz (EpiGear, Version 1.0) for uncertainty analysis (27).
Cost-effectiveness analysis (CEA)
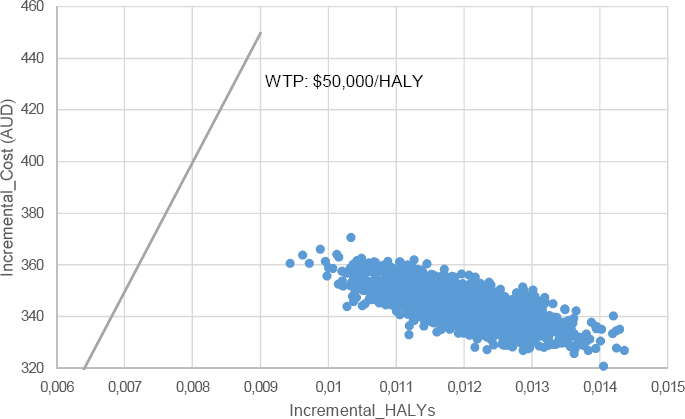
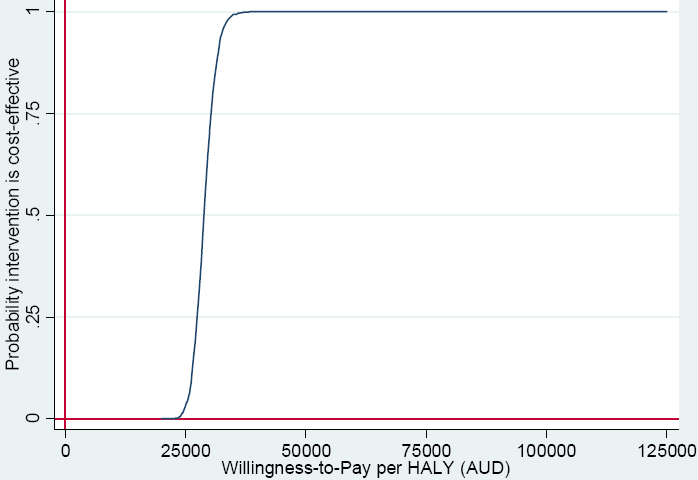
ICER were calculated as cost per life year (LY) gained and costs per health-adjusted life years (HALY) gained. ICER <AU$50 000 per HALY were considered cost-effective in accordance with Australian benchmarks (28). Cost-effectiveness planes are presented to illustrate the incremental differences between groups in costs and benefits. Cost-effectiveness acceptability curves were plotted to show the probability of the intervention being cost-effective at different willingness-to-pay thresholds.
Normal distributions were assumed around the increased time spent standing or being active as a result of the intervention. Univariate sensitivity analyses were conducted to test the following variations in base case assumptions: discount rate of 0% and 6%, and annual decay rate of intervention effect 0% (assuming that the intervention effect would be maintained for 20 years), 10%, 50% and 100%.
Results
Cost efficacy analysis results: within-trial evaluation
Outcomes
Of the 231 participants enrolled and eligible, 204 (86%) completed the 3-month follow-up and 167 (72%) the 12-month follow-up. Participants, at baseline, were aged 24–65 years, with the sample consistently primarily of women (68%), full-time workers (79%), and those categorized as overweight or obese (BMI ≥25kg/m2). Average time at work spent sitting, standing and stepping at baseline were 78.8% (95% CI 76.8–80.9%), 14.3% (95% CI 12.9–15.8%), and 6.9% (95% CI 6.0–7.7%) respectively.
Based on the ITT population, the intervention group significantly reduced workplace sitting by -46.8 (95% CI -69.9– -23.7, P<0.001) minutes/8-hour workday, and overall sitting by -34.8 (95% CI -66.5– -3.1, P=0.032) minutes/16-hour day after 12 months, compared to controls (supplementary table S3, www.sjweh.fi/show_abstract.php?abstract_id=3740). After adjusting for baseline values and confounders, the intervention was not associated with any significant reduction in BMI [0.148 kg/m2 (95% CI -1.407–1.703), P=0.852], quality of life [-0.006 (95% CI -0.074–0.063), P=0.867] or changes in unplanned absences [2.12 days (95% CI -2.01–6.26), P=0.311] relative to controls.
Costs
The pathway analysis for costing intervention delivery is shown in supplementary table S1. The major cost driver was the cost and set-up of the sit-stand workstation (AU$296 per head). The total cost of the intervention was AU$58 570, or AU$431 per participant. In addition, a total cost of AU$4704 or AU$35 per head was incurred over the 12 month period for adverse events attributable to the intervention, mainly for seeking medical treatment from physiotherapists, general practitioners, massage therapists, and osteopaths (supplementary table S2). The per capita cost of the intervention inclusive of adverse events was AU$465.
Cost-efficacy analyses
The incremental cost-efficacy ratio was AU$9.94 ($6.66–$19.63) per minute reduction in workplace sitting time, AU$13.37 ($7.00–150.08) per minute reduction in overall sitting time, and AU$11.02 ($7.68–19.55) per minute increase in workplace standing time, when the costs of treating adverse events were included (table 1). The exclusion of the adverse event costs marginally reduced each of these results.
Table 1
Incremental cost-efficacy results [AE=adverse effect; AU$=Australian dollars; CI=confidence interval].
Uncertainty and sensitivity analyses
The variables having the most effect on the incremental cost-efficacy ratio were consistent between the primary and sensitivity analyses (supplementary table S4, www.sjweh.fi/show_abstract.php?abstract_id=3740). Therefore it was not surprising that when the costs of the sit-stand workstation were not annuitized, the incremental cost-efficacy ratio increased for all three efficacy outcomes. The cost-efficacy results were insensitive to variations in the unit costs of the facilitator/counsellor and the sit-to-stand workstation set-up (regardless of whether costs attributable to adverse events were considered), and to whether the analysis was alternatively based on completers (supplementary table S5, www.sjweh.fi/show_abstract.php?abstract_id=3740).
Cost-effectiveness analysis (CEA) results: modelling of long-term health outcomes and costs
Outcomes
Based on outcomes at 12-months, no significant differences between groups were observed in BMI (or body weight) or workplace stepping time relative to controls (supplementary table S3); however, the difference in workplace standing time was shown to be statistically significant between groups (42.2 minutes/8-hour workday, 95% CI 23.8–60.6, P<0.001). Therefore, changes in activity expressed as standing time (difference in MET between standing and sitting multiplied by the increased standing minutes per week) (29) were modelled. It was assumed that the improvement in activity was fully maintained for the first year, and thereafter decayed at a rate of 20% per annum (ie, after five years, there is no remaining intervention effect).
When modelled for the national population (assuming 624 318 desk-based workers Australia-wide would be affected by the intervention), the intervention resulted in gains of 6243 LY (95% CI 5619–6867) and 7492 HALY (95% CI 6555–8428) [or 0.01 additional LY (95% CI 0.009 – 0.011) and 0.012 HALY for the trial population (95% CI 0.0105 – 0.0135)] (table 2).
Table 2
Base case cost-effectiveness analysis [AU$=Australian dollars; ICER=incremental cost-effectiveness ratio; CI=confidence interval; LY=life years; HALY=health-related quality of life]
| National populationb(AU$) | Trial population (per capita) (AU$) | ICER (AU$) | Cost-effective probability | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Total | Mean (95% CI) | Per participant | Mean (95% CI) | Mean (95% CI) | ||
| Intervention costsa | 269 436 844.46 | 431.57 | ||||
| Cost offsets | -54 403 055.42 (-62 544 159.88– -45 981 007.94) | -87.14 (-100.18– -73.65) | ||||
| Net costs | 215 033 789.04 (206 892 684.58– 223 455 836.52) | 344.43 (331.39– 357.92) | ||||
| LY gains | 6243 (5619– 6867) | 0.0100 (0.0090– 0.0110) | 34 443 (30 126– 39 769) | 100% | ||
| HALY gains | 7492 (6555– 8428) | 0.0120 (0.0105– 0.0135) | 28 703 (24 547– 34 088) | 100% | ||
a The annual average salary of Australia plus the oncost (14%) (accessed from: https://goo.gl/pqiJVT and https://goo.gl/2ebXNw) times the number of states/territory in Australia (inflated to 2014 value via the inflation calculator: http://www.rba.gov.au/calculator/) was added to calculate the total intervention cost.
b Data sourcing from Australian Bureau of Statistics regarding 2014 population size of Australia (accessed from: https://goo.gl/26cREX), employment rate (accessed from: https://goo.gl/8xW5Jj) and physical activity in Australia (accessed from: https://goo.gl/KezM5R) together with the assumption that only 20% of eligible workers would take up the intervention were used to calculate the total costs and benefits if the intervention was implemented at a national level.
Costs
In the trial population, the intervention was associated with cost offsets of -AU$87 (-$100– -$74) (due to the reduced incidence of disease) and a resultant net cost of AU$344 ($331–$358) per participant (table 2).
In the national-level modelling, additional costs of AU$568 375 were incorporated to facilitate coordination of the intervention’s national delivery. The intervention costs totaled AU$269.4 million. Cost offsets of -AU$54.4 million (-$62.5– -$45.9 million) resulted in a total net cost of AU$215 million ($206.8–223.5 million) over the life time of the national cohort, or an average of AU$344 per capita.
Cost-effectiveness
The resultant ICER was AU$34 443 ($30 126–39 769) per LY or AU$28 703 ($24 547–34 088) per HALY gained (table 2), with both having 100% probability of being cost-effective measured against the Australian benchmark of AU$50 000 per LY/HALY (28). The cost-effectiveness plane and cost-effectiveness acceptability curve are shown in figures 1 and 2.
Sensitivity analyses
The assumption around the maintenance of the intervention effect was the key driver of the ICER. If the intervention effect decay rate increased to 50% per year, the intervention became cost-ineffective in terms of cost/LY [AU$57 715 ($51 689–66 202)] and barely cost-effective in terms of cost/HALY [AU$48 721 ($42 183–55 648)] (supplementary table S6 www.sjweh.fi/show_abstract.php?abstract_id=3740). Unsurprisingly, the results were also sensitive to the discount rate assumption.
Discussion
This trial resulted in a robust effect size in terms of the activity change generated by the intervention. The economic evaluation then translated this intermediate outcome observed in the trial (ie, changes in physical activity over 12 months) into final health outcomes (ie, LY and HALY gained over the cohort’s lifetime). The intervention effects were assumed to be sustained for five years only, but the cost relating to the management of avoided diseases were carried forward over the lifetime which are of importance to employers and other stakeholders.
The CEA provides insights relating both to the 231 participants in the Stand Up Victoria intervention trial and to the broader population of desk-based office workers in Australia. It is the first study to report both the within-trial cost-efficacy and long-term cost-effectiveness of an intervention incorporating a sit-stand workstation targeting desk-based workers. Given that society’s willingness-to-pay threshold for a unit exchanged between workplace sitting and standing is unknown, the within-trial cost-efficacy analysis was not able to address the broader economic credentials of this approach. The CEA utilizing the Markov model allowed the translation of the improvement in workplace activity (standing replacing sitting) into long-term health outcomes.
Non-communicable diseases (NCD), particularly cardiovascular disease, cancers, type 2 diabetes and chronic respiratory disease, are dominant global health challenges of the 21st century (30). Underlying most NCD, there are several modifiable behavioral risk factors including physical inactivity and sedentary behavior (31–33); these impose significant cost burdens through increased medical expenditure for treating NCD and through reduced work productivity (34). Given that such costs are incurred by either employers or government, it is of societal interest to identify cost-effective strategies to increase the overall physical activity levels of their constituents. The Markov model employed in the CEA tracked changes in the prevalence and mortality of major NCDs resulting from the decrease in workplace sitting. The intervention delivered gains in LY and HALY, while averting treatment costs due to reduced disease prevalence. If the intervention was maintained (permanent use of sit-stand workstations), there is potential for large gains in life expectancy and healthcare cost savings, given that the current intervention decay effect assumption would be negated. Additionally, the changes in unplanned absences between the intervention period (period 2) and one year after intervention completion suggest a trend (although not statistically significant) for the intervention group participants to lose fewer days than the control group (P=0.311), which warrants further study.
Given that occupational sitting is the single biggest contributor to total weekday sitting time in office workers (35), a sedentary occupation predisposes workers to a heightened risk for weight gain, especially among the physically inactive (33). If this intervention was rolled out to the three million office-based workers Australia-wide (19, 36), and was adopted by (a conservatively estimated) 20%, it would potentially result in a total cost offset of AU$54 million. It may also be more cost-effective than our analysis suggests (AU$28 703/HALY) as the intervention costs could be lowered through modifications of some intervention elements. The cost of the sit-stand workstation (the biggest cost component of the intervention, accounting for 69% of the total intervention cost) could be reduced through economies of scale arising from bulk orders or use of less-expensive models. Sit-stand workstations could also be shared by several workers (eg, among part-time staff) within the same institution. Furthermore, once sit-stand workstations were installed in workplaces, the intervention effect would be potentially maintained (longer than five-year as assumed, provided there was organizational and cultural support for their use), meaning that its economic credentials would be significantly strengthened. In addition, the long-term model does not account for productivity gains in the absence of a disease, which means that the societal savings from the intervention are likely to be substantially underestimated. Other potential savings which could be explored are coaching via text messages rather than the use of health coaches, videos being substituted for seminars, and delivery of the intervention by internal workplace champions. Some of these modifications are already being trialed as part of the BeUpstanding™ program (the scaled-up version of the intervention used in Stand Up Victoria) (37).
Strengths of this cluster RCT include the objectively measured changes in activity time using highly accurate and responsive activity monitoring over 12 months (16). Some study limitations must be acknowledged. Trial participants were recruited from a single organization, which may limit the intervention’s generalizability when scaling up to a larger population. The long-term model only captured changes in BMI and physical activity; this would suggest that the results are probably conservative as there are other cardio metabolic risk biomarkers that showed more promising results (eg, the significant reduction in fasting glucose) (8). Further, the assumption regarding the decay rate of the effect size bears a substantial impact on the cost-effectiveness conclusion. In the absence of any long-term evidence to accurately set the effect decay rate, we adopted an annual rate of 20%, which is conservative compared to that used by others (38).
Concluding remarks
The Stand Up Victoria intervention was shown to be cost-effective when scaled up to the national workforce. Over the lifetime of the cohort of workers, the intervention had a 100% chance of being cost-effective, leading to more LY and HALY gains and lower long-term health costs. Consequently, the Stand Up Victoria intervention to reduce workplace sitting should be considered within any strategies designed to promote the health of the nation’s workforce.